Management of common Obstetric Emergencies
Third and Fourth degree perineal tear
Management of vaginal birth after caesarean
Table of content
1. Severe Pre-Eclampsia
2. Eclampsia
3. Antepartum Haemorrhage
4. Postpartum Haemorrhage
5. Shoulder Dystocia
6. Umbilical Cord Prolapse
7. Anaphylaxis
8. Local Anaesthetic Toxicity
9. TotalSpinal/HighEpidura
10. References
Severe Pre-eclampsia
- Manage as team with Obstetrician, Anaesthetist & Midwife (Refer to Severe pre-eclampsia guidelines on intranet)
- Commence 15-minute MOEWS monitoring RR, pulse oximetry, HR, BP, urine output, temperature Increase frequency if unstable
- IV access and bloods for U+E, LFT, FBC, Clotting, G+S, Urate
- Admit to Maternity critical care unit and commence Maternity critical care unit observation chart
- Commence Magnesium (bolus then infusion) – continue until 24 hours after delivery
- Control BP initially with PO medication
- Control BP with IV anti-hypertensive if not able to control with PO
- Commence arterial BP monitoring
- Fetal monitoring and delivery plan to be decided by obstetricians
- Fluid restrict to 80ml/hr (including all infusions) – Monitor hourly fluid balance
- 6 hourly bloods (U+E, FBC, Clotting, Urate)
- Treat Magnesium toxicity with 10ml 10% calcium gluconate
Drug doses and cautions
- Magnesium LOADING DOSE: 4g (in 50ml pre-mixed bag) Give over 5-10 minutes – rate 300-600ml/hr
- MAINTENANCE: 1g / hour (in 250ml pre-mixed bag) Rate 10ml/hr
- Monitor: Respiratory Rate & O2 saturation, hourly urine output and 4 hourly patella reflex – Do not routinely monitor magnesium levels
Labetalol (1st choice)
- Contraindication: Severe asthma
- Caution: Cardiac disease
- Per oral dose: 200mg – repeated after 30 mins
- IV Bolus: 50mg (10mls of 5mg/ml) given over at least 5 mins – repeat dose every 10mins (maximum 200mg)
- IV Infusion (5mg/ml preparation): Commence at 4 ml/ hr – double every 30 mins to maximum of 32 ml/hr until BP stable
- If BP not <160/105 after 90 mins or if SBP >160mmHg despite 32ml/hr add in second line agent
Nifedipine modified release
- Per Oral dose: 10mg capsules 4-6hrly
Hydralazine IV Bolus:
- 2.5mg IV over 5 mins – repeat at 20 min intervals as required to max 20mg.
- Monitor BP every 5 mins. If required consider infusion.
- IV infusion: 40mg in 40mls normal saline (1-5ml/hr)
Eclampsia
- Pull emergency buzzer Summon Consultant Obstetrician and Consultant Anaesthetist to attend immediately
- Turn patient to left lateral position
- Assess and maintain airway
- Apply oxygen 15L/min via non-rebreathe mask
- Secure IV access and take blood (FBC, U+E, Clotting, G+S, blood sugar)
- Give Magnesium BOLUS dose (4g IV over 5-10 mins)
- Start Magnesium MAINTENANCE infusion 1g/hr (10ml/hr)
- If fit not terminated / patient fits again: Repeat magnesium bolus 2g bolus (or 4g bolus if booking weight >70Kg) over 5-10 mins Increase infusion to 1.5g/hr (rate 15ml/hr)
- Obstetrician to make plan for fetal monitoring and delivery
- Resistant seizures may require general anaesthesia ± anticonvulsants (refer to Trust guidelines; involve Anaesthetist)
- Consider other causes of seizure
Drug doses and cautions
Magnesium
LOADING DOSE: 4g (in 50ml pre-mixed bag)
Give over 5-10 minutes – rate 300-600ml/hr
Persistent / repeated fits: Repeat as for normal loading dose if booking weight >70kg
If booking weight <70kg: Give 25ml (half) of 50ml pre-mixed bag at 150-300ml/hr
MAINTENANCE: 1g / hour (in 250ml pre-mixed bag)
Rate 10ml/hr
Persistent / repeated fits: increase rate to 15ml/hr (1.5g/hr)
Considerations-Consider other causes of seizure
- Hypoglycaemia (check BM)
- Epilepsy (past medical history)
- Drugs (prescribed and recreational)
- Intra-cerebral bleed (check for other signs)
Antepartum Haemorrhage
Bleeding from or into the genital tract, from 24+0 weeks onwards and prior to the birth of the baby
- Pull emergency buzzer Summon Obstetrician and Anaesthetist to attend immediately
- Record all vital signs and calculate MEOWS
- Apply 15L/min oxygen via non rebreathe mask
- Cannulate with wide bore cannula – Take bloods for FBC, clotting and X-match 4 units of blood (send samples to lab by hand, not pod)
- Send Kleihauer if mother is Rhesus D negative
- Commence IV fluids 1000ml Hartmann’s solution
- Assess her pain: If continuous – consider abruption If with contractions – consider labour
- Palpate the abdomen
- Listen for fetal heart +/- commence CTG (depending on gestation)
- Perform a speculum examination: Assess cervical dilatation Visualise lower genital for cause of APH
- Do a VE if labour suspected – NOT if placenta praevia suspected
Considerations
- Activate Major Obstetric Haemorrhage Protocol if: Over 1.5L blood loss with ongoing loss Ongoing blood loss with haemodynamic instability
- Alert: Consultant Obstetrician and Consultant Anaesthetist (must be informed) Theatre staff (if not already in attendance) Coordinator to liaise with Blood Bank staff
- Consider: Tranexamic acid 1g IV, Cell salvage
Postpartum Haemorrhage PPH
Blood loss >500ml within 24hrs of delivery; Major >1.5L, Massive >2,5L
- Pull emergency buzzer Summon Obstetrician and Anaesthetist to attend immediately
- Request PPH trolley
- Apply oxygen 15L/min via non-rebreathe mask
- Secure 2 x IV access (grey cannula if possible) – Take blood for FBC, U+E, Clotting, Fibrinogen and X-match 4u
- Commence IV fluids 1000ml Hartmann’s solution
- Record all vital signs and calculate Modified Obstetrics Early Warning Score MOEWS
- Establish source of bleeding ASSESS 4 T’s: Tone, Trauma, Tissue, Thrombin
- If atonic uterus: Rub up a contraction Insert urinary catheter
- Commence drug algorithm for uterine atony (see appendix A below)
- Consider bimanual uterine compression
- Consider Examination Under Anaesthesia in theatre
- Consider Bakri balloon insertion
- 2 units O negative blood are in Blood Fridge
- Activate the Major Obstetric Haemorrhage Protocol
- Weigh all swabs – Document swab count (on board & in notes
(Appendix A) Uterine atony drugs and cautions
- Syntometrine (IM) can be repeated if used at time of delivery (avoid if ↑BP)
- Ergometrine can be given if syntometrine not used (avoid if ↑BP)
- Syntocinon 2nd bolus of 5iu
IV Infusion – 30iu in 500ml 0.9% saline at 150ml/hr
- Haemabate 250mcg IM repeated every 15 mins maximum 8 doses (avoid if asthmatic) Misoprostol 1000mcg (5 x 200mcg tablets) PR
- Administer tranexamic acid 1g IV
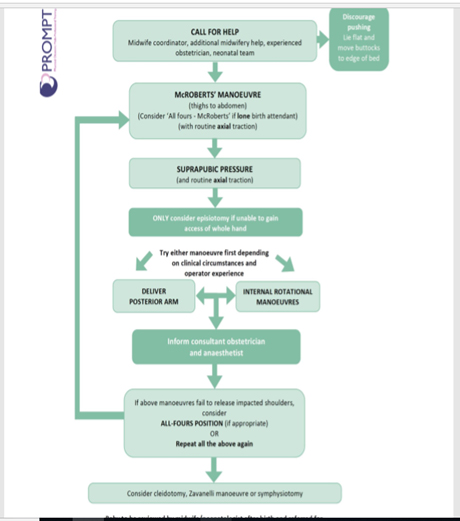
Shoulder dystocia
- Pull emergency buzzer -Summon Obstetrician, Midwifery Coordinator, Neonatal team and Anaesthetist
- Advise the woman to STOP pushing
- Lie flat with tilt – move buttocks to end of bed
- Follow FLOWCHART OVERLEAF for manoeuvres
- Only use routine axial traction – do not pull downwards
- If manoeuvres have failed, you must inform the Obstetric Consultant
Umbilical cord prolapse
- Pull emergency buzzer Call for Obstetrician, Midwifery coordinator, Neonatal team and Anaesthetist
- Do not handle the cord (if possible)
- If second stage and parous: Expedite immediate vaginal delivery for maternal / neonatal safety-Consider instrumental delivery
- Manually elevate presenting part or fill the bladder
- Encourage into the following position: Left lateral Head down with a pillow placed under left knee or knee to chest position
- Ensure continuous fetal monitoring (if not already in place)
- Consider tocolysis Terbutaline 250 mcg subcutaneous or GTN spray 2 puffs sublingual
- Emergency transfer to Delivery suite
- Assess and assist birth by quickest means
- Urgency of birth dependent on Fetal Heart rate and gestational age
- If emergency caesarean section required, spinal may not be appropriate – Discuss with anaesthetist
Determining fetal viability
- If the cord is not pulsating at the time of the INITIAL examination: Ascertain by ultrasound whether a fetal heartbeat is present
- If the fetus is no longer alive – vaginal delivery should be facilitated
- If the fetal heart has definitely been recorded within the preceding 5 minutes – consider category 1 caesarean section
Anaphylaxis
Symptoms include: hypotension, tachycardia, wheeze, rash, swelling, altered mental state
- Pull emergency buzzer Summon the Anaesthetist and Obstetrician
- Remove potential causative agents (e.g. antibiotics, gelofusine, latex, chlorhexidine)
- Apply oxygen 15L/min via non-rebreathe mask
- Lie patient flat with tilt and elevate legs
- Give Adrenaline: IM 0.5ml of 1:1000 (small ampoule) – repeat PRN
Anaesthetists only may give IV adrenaline
-50mcg (0.5ml of 1:10,000) titrated to response
-An infusion may be needed
- IV access and take blood – FBC, clotting, G+S, mast cell tryptase
- Commence IV fluids 1000ml Hartmann’s solution
- Record all vital signs and calculate MOEWS
- Obstetrician to make plan for fetal monitoring and delivery
- Administer chlorphenamine 10mg IV (or IM)
- Administer hydrocortisone 200mg slowly IV (or IM)
- Treat persistent bronchospasm (with inhaled/IV salbutamol, IV aminophylline or magnesium sulphate)
- Summon ICU Anaesthetist – consider arterial and central lines
Drug doses and treatments
- IM Adrenaline 1:1000 0.5ml repeat every 5 mins until improvement
- IV Adrenaline bolus – ANAESTHETIST ONLY 50mcg bolus (0.5ml 1:10 000 minijet) titrated to response
- IV Adrenaline infusion 4mg adrenaline in 50ml 5% dextrose Infuse at 5-10ml/hr (approx. 0.05-0.1mcg/kg/min)
- Salbutamol 2.5mg via oxygen driven nebuliser or 250mcg slow IV
- Aminophylline 250mg slow IV
- Magnesium sulphate 2g IV over 20 mins
Serial Tryptase
Send blood for Tryptase in red top bottle Immediately, at 2 hours and at 24 hours
Local Anaesthetic toxicity
May occur distant to initial injection. Signs include: Sudden alteration in mental state (agitation/loss of consciousness/fit) Cardiovascular collapse, bradycardia, heart block, arrhythmias, arrest
- Stop local anaesthetic infusion / injection
- Pull emergency buzzer – Note the time Summon the Anaesthetist (if not present) and Obstetrician Request the Adult Resuscitation Trolley
- Assess airway & apply O2 15L/min via non-rebreathe mask Tracheal tube maybe needed to secure airway Hyperventilation may help increase blood pH
- Attach ECG monitoring (3 lead or use defibrillation pads)
- Record all vital signs and calculate MOEWS
- Secure IV access and commence 1000ml Hartmann’s solution
- Control seizures: Use benzodiazepines, thiopentone &/or propofol
- Commence intralipid: Initial bolus then commence infusion (see overleaf) Repeated boluses & increased infusion rate may be required Use standard ALS algorithms for management of resuscitation
- Obstetrician to make plan for fetal monitoring and delivery
- Note that resuscitation may take considerable time (>1hr)
Drug doses and treatment
Intralipid 20%
- Initial bolus 1.5ml/kg over 1minute
- Commence infusion 15ml/kg/hour
- If cardiovascular instability after 5 minutes-Repeat bolus and increase infusion to 30ml/kg/hour
- If cardiovascular instability after another 5 minutes- Final bolus 1.5ml/kg Give maximum of 3 boluses
Do not exceed maximum cumulative dose 12ml/kg
Follow up
- Monitoring until sustained recovery achieved
- Exclude pancreatitis
- Regular clinical review
- Daily amylase for 2 days
- Report case to NPSA National patient safety agency
- Report use of intralipid to www.lipidregistry.org
High Epidural block/Total Spinal
Block of T4 or higher or regional block with adverse signs, including: Cardiovascular collapse with hypotension & bradycardia, difficulty in breathing, tingling/numbness in hands, reduced consciousness
- Stop epidural infusion
- Pull emergency buzzer Summon Anaesthetist and Obstetrician to attend immediately
- Apply oxygen 15L/min via non-rebreathe mask
- Secure IV access – Take bloods for FBC, U+Es, G+S, lactate
- Commence IV fluids 1000ml Hartmann’s solution
- Record all vital signs and calculate MOEWS
- Position of patient depends on haemodynamic stability: Sit patient up if able to tolerate In case of collapse, lie patient flat with left lateral tilt / uterine displacement
- If airway and breathing compromised or patient unconscious – proceed to intubate and ventilate
- Treat bradycardia with 500mcg atropine bolus (max 3mg)
- Treat hypotension with vasopressors / adrenaline
- Exclude other causes of hypotension
- Obstetrician to make plan for fetal monitoring and delivery
Drug doses and treatment
- For hypotension consider vasopressors/ionotropes: Ephedrine 6mg bolus, Phenylephrine 100mcg bolus, Metaraminol 500mcg bolus
- For bradycardia: Atropine 500mcg to maximum 3mg
Consider other causes of hypotension
- Bleeding
- Sepsis
- Local anaesthetic toxicity
- Anaphylaxis
References
Royal Bolton Hospital template for Obstetric emergencies
