Venous thromboembolism prophylaxis
Management of vaginal birth after caesarean
Acute management of thromboembolism disease in pregnancy and puerperium
Venous thromboembolism prophylaxis
Table of content
1. Background
2. Risk factors in pregnancy and puerperium
3. Risk stratification
4. First trimester risk factors
5. Thrombophilia
6. Asymptomatic heritable thrombophilia
7. Previous recurrent VTE
8. Previous VTE
9. Family history
10. Low molecular weight heparin and delivery
11. Management algorithm
Background
- Low molecular weight heparin reduces the risk of medical and surgical venous thromboembolism by 60% and 70% respectively
- Incidence of pulmonary embolism in maternity is 1.3 in 10,000
- Heritable thrombophilia is found in 20-50% of pregnancy related venous thromboembolism
- Patient with previous VTE have a recurrence risk of 2-11% (OR 25)
- Hospital admission increases VTE risk by 18-fold
- There is a 6-fold increase in VTE 28days post discharge
- Risk of VTE is higher if admission is >3days-If <3days there is a 4-fold increase, if >3days there is 12-fold increase
Risk factors in pregnancy and puerperium
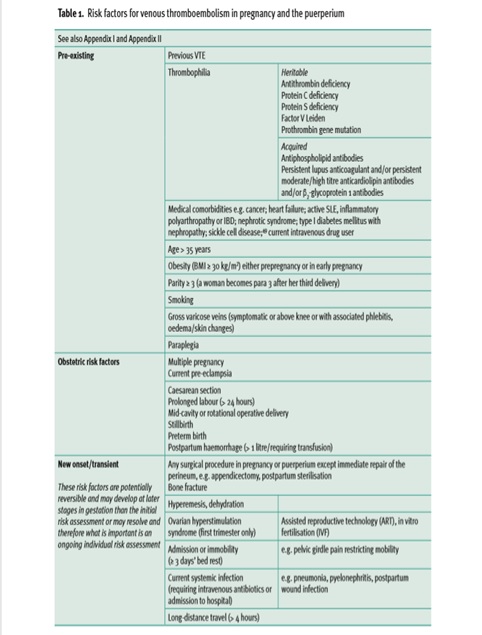
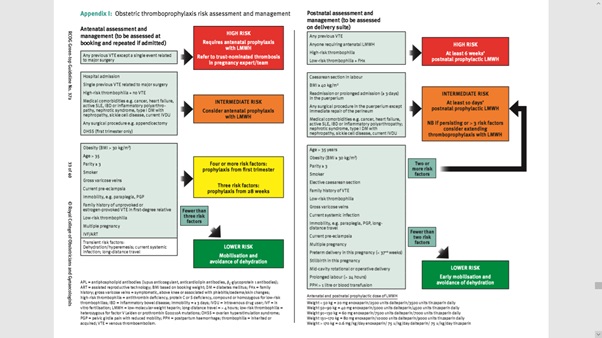
Risk stratification
- 4 or more risk factors offer low molecular weight heparin (LMWH) antenatally till 6weeks postpartum
- 3 risk factors offer LMWH from 28weeks gestation till 6weeks postpartum
- 2 risk factors offer LMWH 10 days postpartum
First trimester risk factors
- Women admitted with hyperemesis should be considered for thromboprophylaxis with LMWH and can discontinue thromboprophylaxis when the hyperemesis resolves.
- Women with ovarian hyperstimulation syndrome should be considered for thromboprophylaxis with LMWH in the first trimester.
- Women with an IVF pregnancy and three other risk factors should be considered for thromboprophylaxis with LMWH starting in the first trimester.
Thrombophilias
Previous VTE associated with Antithrombin deficiency or Antiphospholipid syndrome (Usually on oral anticoagulant)
- Start on 50%, 75% or full treatment dose of LMWH antenatally
- Continue for 6 weeks postpartum or till oral anticoagulant
- Monitor Anti-Xa levels (Aim for 4-hour peak level of 0.5-1.0IU/ml)
Asymptomatic heritable thrombophilia
Women with asymptomatic antithrombin, protein C or S deficiency or those with more than one thrombophilic defect (including homozygous factor V Leiden, homozygous prothrombin gene mutation and compound heterozygotes) should be
- Referred to a local expert and antenatal prophylaxis considered.
- Administer six weeks’ postnatal prophylaxis even in the absence of additional risk factors
Previous recurrent VTE
- May require higher Prophylactic LMWH doses
- If on Warfarin-Change to LMWH as soon as pregnancy is confirmed
-Within 2 weeks of missed period
-Before 6 weeks
- If not on warfarin commence LMWH ASAP
Previous VTE
- Related to thrombophilia-manage as above i.e. patient with thrombophilia
- Unprovoked or oestrogen related e.g. combined oral contraceptive-Antenatal LMWH+6weeks postpartum
- VTE provoked by major surgery give LMWH from 28weeks + 6weeks postpartum
Family history
- Consider thrombophilia testing if women with no risk factor have a family history of unprovoked or oestrogen provoked VTE in a first degree relative < 50years
LMWH and delivery
- Avoid spinal/epidural for 12 hours after prophylactic LMWH and 24 hours after treatment dose
- Stop LMWH once labour begins
- No LMWH for 4hours post spinal/epidural
- Do not remove epidural until 12 hours from last LMWH
- Omit LMWH on the morning of elective CS
- Administer LMWH 10 days post-delivery after caesarean section
- If no risk of Postpartum haemorrhage-start immediately after normal delivery provided patient had no epidural or spinal
- If risk of postpartum haemorrhage-Delay start of LMWH or consider unfractionated heparin
- If bleeding occurs while on LMWH – stop LMWH and seek expert advice
- Women at high risk of haemorrhage with risk factors including major antepartum haemorrhage, coagulopathy, progressive wound haematoma, suspected intra-abdominal bleeding and postpartum haemorrhage may be managed with anti-embolism stockings (AES), foot impulse devices or intermittent pneumatic compression devices. Unfractionated heparin (UFT) may also be considered
RCOG-Algorithm for risk assessment and management
Reference
- Thrombosis and Embolism during pregnancy and puerperium, reducing the risk (Green top guideline No. 37a)a
