Menopause and Hormone replacement therapy
Management of breech presentation
Parvovirus infection in pregnancy (Slapped Cheek syndrome)
Menopause And Hormone Replacement Therapy
Dr Funmi Odusoga DFRSH MRCOG
Table of content
1. Definition
2. Incidence/Epidemiology
3. Physiological effect of menopause
4. Management
5. Information for General practitioners
6. Which HRT regimen
7. Long term benefit and Risk
8. Premature ovarian Insufficiency
9. Reference
Definition
- Menopause-Cessation of menstrual period for 12 months or more
- It marks the end of a woman’s reproductive capacity
- Premenopausal-means before menopause
- Post menopause- means after menopause
- Climacteric/Perimenopausal period –It is the transition period during which the woman’s reproductive function gradually diminishes and disappears
Incidence / Epidemiology
- Mean age is 51yrs
- 97% of women are menopausal by 58years
- 0.3-0.9% are menopausal before 40years (Premature Ovarian failure)
- Gene not yet found
- Socioeconomic status (lower is linked to earlier earlier)
- Higher parity is linked to Late menopause
- Smoking is linked to early menopause
Diagnosis
- Women aged over 45 -Perimenopause is diagnosed based on vasomotor symptoms and irregular periods not with blood test as hormone levels are erratic and unpredictable
- Menopause is diagnosed in women who have not had a period for at least 12 months and are not using hormonal contraception
- Menopause diagnosis is based on symptoms in women without a uterus
Clinical Features Of Perimenopause
- Lasts between 2-5 years
- Changing period, mood swings, low self-esteem, vasomotor symptoms headache, premenstrual syndrome, insomnia, palpitations, tiredness, irritability, poor concentration, poor cognitive function, foggy head, difficulty in making decisions
Physiological Effect of Menopause
- Cardiovascular-Increased Cardiovascular risk
- Endometrium-Bleeding problems
- Musculoskeletal-Joint and muscle ache, Osteoporosis (remember importance of detection, prevention & treatment)
- Brain-Memory & Cognition difficulties
- Vasomotor symptoms-night sweats, hot flashes, flushing
- Urogenital -Vaginal atrophy, Urinary symptoms and Sexual problem
Management
- Individualised care-Identify and manage patients need
- Do not do Anti Mullerian Hormone, inhibin A or B, oestradiol, antral follicle count, ovarian volume to diagnose perimenopause or menopause in women over age 45. Manage patients symtomatically
- Do not check Follicle Stimulating Hormone (FSH) if on Combined Oral Contraceptives or high dose progestogen
- Check FSH only in women aged 40-45 with symptoms including change in menstrual cycle and in women aged under 40 with menopausal symptoms
Information For General Practitioner / Specialist
- Explain stages of menopause, common symptoms, lifestyle changes and intervention, benefit and risk of treatment, long term health implication of menopause
- Information about types of treatment, HRT, non-hormonal e.g. Clonidine, non pharma, Cognitive behavioural therapy
- Offer information to women who are likely to go through menopause due to surgical and medical intervention.
- Refer to Menopause specialist if in doubt
Lifestyle Intervention
- Loose cotton layers
- Fans
- Avoid spicy foods
- Avoid hot drinks especially caffeine
- Reduce alcohol intake
- Stop smoking
- Increase exercise
- Lose weight
- Improve glucose tolerance
Management Of Abnormal Bleeding
- Obtain endometrial lining biopsy if indicated on scan
- Tranexamic and mefenamic if periods are more frequent
- Progestogen is useful for irregular cycle, give longer than the luteal phase ( Beware or norethisterone , Medroxyprogesterone is better)
- Mirena- you can add estrogen
- COCP is underrated but useful (Check UK medical eligibility criteria)
- Consider extended pill regimen
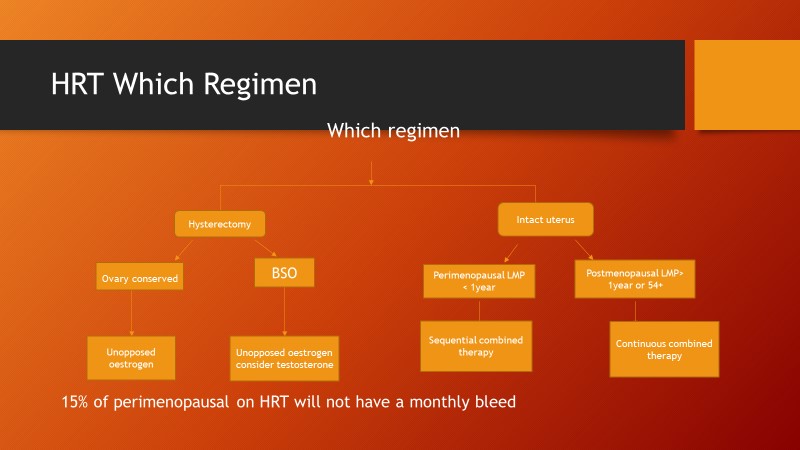
Regimen (see chart above)
- For patient requiring unopposed oestrogen give oestrogen from day1 to day 28
- For sequential combined therapy- oestrogen is given from day 1 to day 28, progestogen is given from day 14 to day 28
- For continuous combined oestrogen and progesterone are given from day 1 to day 28
Managing Short Term Symptoms
❑ Vasomotor-Oestrogen and progesterone to women with uterus
❑ Oestrogen alone to women without a uterus
❑ SSRIs, SNRIs and clonidine should not be used as 1st line treatment
❑ Isoflavone and black cohosh-
- Beware as safety is uncertain
- Different preparation may vary
- May interact with other drugs
Psychological Symptoms
- Give HRT to alleviate low mood that arises as a result of the menopause
- Offer Cognitive behavioural therapy for low mood & Anxiety
- There is no clear evidence for SSRIs and SNRIs if not diagnosed with depression
Altered Sexual Function
❑ Consider Testosterone
Urogenital Atrophy
- Vaginal oestrogen- even if they are on systemic HRT
- If systemic HRT is contraindicated seek advice from menopause expert
Complimentary Therapy And Unregulated Preparations
- Efficacy and safety of unregulated compounded bioidentical hormones are unknown
- St John wort may relief vasomotor symptoms but there is uncertainty about dosage,variation in nature and potency, persistence of effect, interaction with drugs e.g. tamoxifen, anticoagulant and anti-convulsant
Review And Follow Up Of Women On HRT
- Women must keep up to date with national health screening
- Review treatment 3 months after commencing HRT to assess efficacy and tolerability
- Review patient Annually
- Refer to specialist if no improvement of symptoms or side effects or contraindications to HRT
- Unscheduled bleeding is common side effect within 3 months of treatment and should be reported at 3-month review. If bleeding occurs after 3 months refer for endometrial screening
Stopping HRT
Gradually reducing may limit recurrence of symptom in short term but makes no difference in the long term
Women With High Risk Of Breast CA
- Refer women to specialist (Gynaecologist with special interest in managing menopause)
- Do not offer SSRIs
Long Term Benefits And Risk
- Venous Thromboembolism- risk of HRT is greater in oral than transdermal
- Consider transdermal if BMI >30
- Refer to haematologist if high risk of Venous thromboembolism, strong family history or hereditary thrombophilia
Cardiovascular
- Does not increase CVS risk in women <60
- Does not affect risk of dying from CVS disease
- HRT with oestrogen is associated with no or reduced risk of coronary heart disease
- Oestrogen and progesterone has little or no increase in risk of coronary heart disease
- Oral but not transdermal is associated with small increase in the risk of stroke.
- Diabetes- HRT does not have adverse effect on blood glucose control
Breast CA
- Oestrogen alone –little or no change in risk of breast ca
- Oestrogen and progesterone-Increase in risk of breast CA
- Increase in risk is reduced after stopping HRT
Osteoporosis
Risk of fragility fracture is decreased whilst taking HRT
Dementia
❑ It is not known f HRT affects the risk of dementia
Colorectal
Reduces risk
Premature Ovarian Insufficiency
Cessation of periods due to ovarian failure under 40 years
Aetiology
Most are idiopathic
- Take into account previous medical (10-30% have concurrent autoimmune disease such as hypothyroidism), surgical(previous oophorectomy/endometrioma) and family history (5-30%) have another affected relative
- Associated with fragile X, turner’s and down syndrome
- Associated with Chemotherapy, radiotherapy or ischaemia after uterine artery embolisation
Diagnosis
- (Under 40)
- Infrequent or no periods
- Elevated FSH levels on 2 blood samples taken 4-6 weeks apart. FSH>30IU and high LH
- Chromosomal analysis and autoimmune screening may help to identify underlying causes
Management Of Premature Ovarian Insufficiency
- COCP or HRT except contraindicated e.g. women with hormone sensitive Cancer
- Continue to age 50
- HRT may have beneficial effect on BP compared with COCP
- HRT/COCP offer bone protection
- HRT should not replace effective contraception as unpredictable spontaneous return of ovarian function does occur in a few women
- Dual X-ray absorptiometry should be arranged for a baseline bone density measurement
Side Effect Of Systemic HRT
- Oestrogen related- fluid retention, bloating, breast tenderness or enlargement, nausea, headaches, leg cramps and dyspepsia
- Progestogen related- fluid retention, breast tenderness, headaches or migraines, mood swings, depression, acne, lower abdominal pain, backache.
- Combined – irregular, breakthrough bleeding.
- All types- weight gain
Reference
- NICE guideline November 2015
