Diabetes in pregnancy
Asthma in pregnancy
Fibroid (Leiomyoma)
Diabetes in Pregnancy
Dr Ayesha Ajmi
Table of content
1. Physiological changes
2. Classification
3. Incidence
4. Effect of pregnancy on diabetes
5. Effect of pre-existing diabetes on pregnancy
6. Management
7. Risk factors for gestational diabetes
8. Antenatal care
9. Postnatal cares
10. References
Physiological changes
- In the last trimester there is a state of physiological insulin resistance and glucose intolerance
- Altered glucose handling i.e. fasting level decreases and post prandial increases
- Glucose tolerance decreases with increasing gestation after the first trimester; largely due to the anti-insulin hormones secreted by the placenta; human placenta lactogen, glucagon and cortisol
- Normal women show approximate doubling of insulin production from end of first trimester to third trimester
- These changes causes increased insulin requirement in established diabetes and development of abnormal glucose tolerance in gestational diabetes, where there is insufficient insulin secretion to compensate for insulin resistance
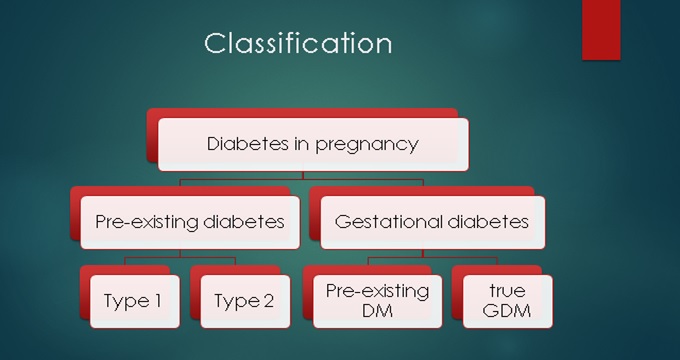
Classifications
Incidence in the United Kingdom
- The prevalence of type 1 is about 0.5% and that of type 2 about 3%–4% (lower in women of childbearing age, but higher in Afro-Caribbean and 10% in Asian immigrants)
- The prevalence of pre-existing diabetes in pregnancy in the United Kingdom is about 0.4% (0.27% type 1 and 0.1% type 2)
Effect of Pregnancy on diabetes
- Women with type 1 diabetes require increasing doses of insulin as pregnancy progresses
- Maximum requirements at term is twofold pre-pregnancy dose
- Women with type 2 DM require addition of insulin to therapy or increase in insulin dose
- There is rapid increase in insulin requirement between 28-32 weeks when fetus is rapidly growing.
Diabetic nephropathy
- Deterioration in renal function and particularly proteinuria
- Deterioration in renal function may be irreversible and this is more likely in moderate to severe renal impairment; i.e. Chronic Kidney Disease stage 3-5, creatinine >125 μmol/L pre-pregnancy and hypertension
- Refer to nephrologist if creatinine > 120 or proteinuria >2g/day
- Deterioration in mild renal impairment is reversible
Diabetic retinopathy
- Two fold risk of progression of diabetic retinopathy
- May start in pregnancy
- Rapid improvement in glycaemic control (feature of first trimester) and increase in retinal blood flow
- Risk is higher for type 1DM
- Related to poor metabolic control, diastolic hypertension, renal disease, anaemia and severity of baseline retinopathy
Hypoglycaemia
- Hypoglycaemia is more common in pregnancy (largely related to intensified diabetic control) and may be associated with relative ‘hypoglycaemia unawareness’
- Most maternal deaths in the United Kingdom caused by diabetes are due to hypoglycaemia
- For every 1% fall in HbA1C, there is a 33% increase in hypoglycaemic attacks
Other effects
- Diabetic ketoacidosis is rare (1%–3%) in pregnancy, probably in part related to the close supervision, but is a risk in the presence of hyperemesis, infection or corticosteroid therapy
- Women with autonomic neuropathy and gastric paresis may experience worsening of symptoms
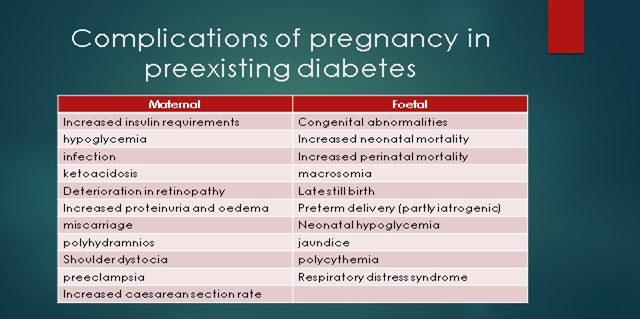
Effect of pre-existing diabetes on pregnancy
- Increased risk of miscarriage
- 3 to 4 fold increased risk of preeclampsia; further increased by renal disease and hypertension and this is related to glycaemic control
- 1% increment in HBA1C increases risk by 60%
- Pregnancies in women with diabetic nephropathy are often complicated by severe oedema related to proteinurea and hypoalbuminaemia and normochromic normocytic anaemia
- Infections: UTI, respiratiory, endometrial, wound
- Caesarean section is increased to about 65%
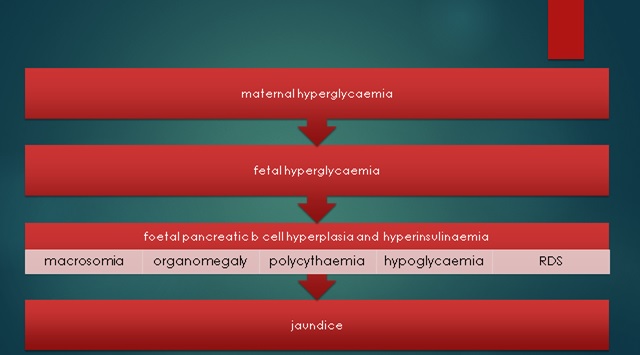
Foetal Considerations
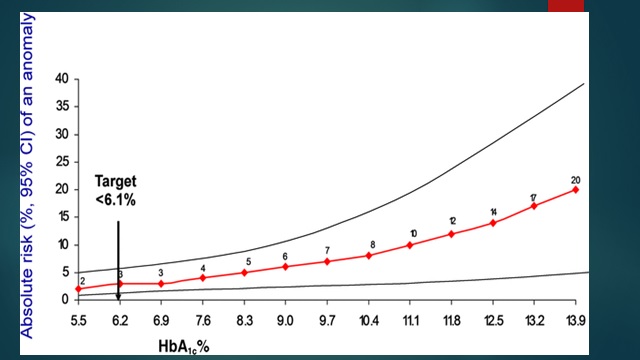
- Risk of congenital abnormalities 4% (double background)
- Congenital abnormalities is related to HbA1c at conception; 25% risk if >10%; eliminated if HBA1C normal
- Increased risk of sacral agenesis, congenital heart defect, neural tube defect, skeletal abnormalities
- Perinatal and neonatal mortality increased to 5-10 fold; again related to HBA1C at conception
- Sudden unexplained Intra Uterine Death after 36 weeks; related to diabetic control
- Fetal hyperinsulinaemia may lead to chronic fetal hypoxia, which in turn stimulates extramedullary haemopoiesis, fetal polycythaemia and neonatal jaundice
Management
Pre-pregnancy counselling- Discuss and advise patient on
- The role of diet, body weight and exercise
- The risks of hypoglycaemia and impaired awareness of hypoglycaemia during pregnancy
- How nausea and vomiting in pregnancy can affect blood glucose control
- The increased risk of having a baby who is large for gestational age, which increases the likelihood of birth trauma, induction of labour and caesarean section
- The need for assessment of diabetic retinopathy before and during pregnancy
- The need for assessment of diabetic nephropathy before pregnancy
- The importance of maternal blood glucose control during labour and birth and early feeding of the baby, in order to reduce the risk of neonatal hypoglycaemia
- The possibility of temporary health problems in the baby during the neonatal period, which may require admission to the neonatal unit
- The risk of the baby developing obesity and/or diabetes in later life.
- Aim for HbA1c <6.5%, avoid pregnancy if >10%
Risk factors for gestational diabetes
Offer GTT if at booking:
- BMI above 30 kg/m2
- Previous macrosomic baby weighing 4.5 kg or above
- Previous gestational diabetes
- Family history of diabetes (first‑degree relative with diabetes)
- Minority ethnic family origin with a high prevalence of diabetes.
- Do not use fasting plasma glucose, random blood glucose, HbA1c, glucose challenge test or urinalysis for glucose to assess risk of developing gestational diabetes. Offer testing if 2+glycosuria or 1+ on 2 or more occasions
Importance of Gestational Diabetes mellitus (GDM)
- Increased risk (40-60%) of developing type 2 DM within 10-15 years
- Diagnosis of type 2 often delayed and 10-30% have established renal or eye disease at diagnosis
- Modification of diet and lifestyle with correction or avoidance of obesity may prevent or delay diabetes later in life
- 1:1000 will have diabetes predating pregnancy; at risk of all features of pre-existing diabetes
- Macrosomia and adverse pregnancy outcomes
- GDM is diagnosed by National Institute for Clinical Excellence with fasting blood sugar of 5.6mmols/l or above and above and 75g 2hours OGTT of 7.8mmol/litre or above
- There is a varied criteria for screening in different hospitals
Intervention
- Refer to Joint Antenatal clinic/Diabetes within 1 week
- Good glucose control reduces risk of fetal macrosomia, trauma during birth, induction of labour and/or caesarean section, neonatal hypoglycaemia and perinatal death
- Self-monitoring of blood glucose
- Advise changes in diet and exercise
- Foods with lower glycaemic index
- Refer to dietician
- Exercise- walking for 30 min after a meal
- Offer trial of diet and exercise if fasting <7
- Offer metformin if blood glucose targets not met within 1-2 weeks
- Addition of insulin should be considered if poor control with metformin
- Offer immediate insulin if fasting >7 or fasting 6-6.9 with macrosomia or hydramnios
- Consider glibenclamide in women who decline insulin or cannot tolerate metformin
- 10-20% of women with GDM will need oral hypoglycaemic or insulin therapy
Pattern of action of short acting insulin
- Onset: within 0.5 hours.
- Maximum effect: 1.5 hours then steep decrease to zero by 5.5 hours.
- Duration: 5.5 hours
Pattern of action of long acting insulin
- Onset: within 1.5 hours.
- Maximum effect: 4–12 hours, then steady decrease in levels.
- Duration: 24 hours
Insulin pump
- NICE currently recommends their use if glycaemic control cannot be controlled by multiple daily injections without significant hypoglycaemia.
- Continuous glucose sensors use a subcutaneous probe to continually assess interstitial glucose levels.
Blood sugar target
- Fasting – 5.3
- 2 hours – <7.8
Antenatal care
- Booking appointment (joint diabetes and antenatal care) – ideally by 10 weeks
- Discuss information, education and advice about how diabetes will affect the pregnancy, birth and early parenting
- Discuss importance of achieving optimal blood glucose control, avoiding hypoglycaemia
- Review medicines for diabetes and its complications.
- Offer retinal assessment for women with pre‑existing diabetes unless the woman has been assessed in the last 3months
- Offer renal assessment for women with pre‑existing diabetes if this has not been performed in the last 3months
- Arrange contact with the joint diabetes and antenatal clinic every 1–2 weeks throughout pregnancy for all women with diabetes.
- Measure HbA1c levels for women with pre‑existing diabetes to determine the level of risk for the pregnancy.
- Offer self‑monitoring of blood glucose or a 75g 2‑hour OGTT as soon as possible for women with a history of gestational diabetes who book in the first trimester.
- Confirm viability of pregnancy and gestational age at 7–9 weeks.
16weeks
- Offer retinal assessment at 16–20 weeks to women with pre‑existing diabetes if diabetic retinopathy was present at their first antenatal clinic visit.
- Offer self‑monitoring of blood glucose or a 75g 2‑hour OGTT as soon as possible for women with a history of gestational diabetes who book in the second trimester.
20weeks
- Offer an ultrasound scan for detecting fetal structural abnormalities, including examination of the fetal heart (4 chambers, outflow tracts and 3 vessels).
28weeks
- Offer ultrasound monitoring of fetal growth and amniotic fluid volume.
- Offer retinal assessment to all women with pre‑existing diabetes.
- Women diagnosed with gestational diabetes as a result of routine antenatal testing at 24–28 weeks enter the care pathway
32 weeks
- Offer ultrasound monitoring of fetal growth and amniotic fluid volume.
- Offer nulliparous women all routine investigations normally scheduled for 31 weeks in routine antenatal care.
34 weeks
- No additional or different care for women with diabetes.
36 weeks
- Offer ultrasound monitoring of fetal growth and amniotic fluid volume.
- Provide information and advice about timing, mode and management of birth analgesia and anaesthesia changes to blood glucose‑lowering therapy during and after birth
- Discuss care of the baby after birth
- Discuss initiation of breastfeeding and the effect of breastfeeding on blood glucose control
- Discuss contraception and follow-up
37 to 38 + 6 weeks
- Offer induction of labour, or caesarean section if indicated, to women with type 1 or type 2 diabetes
- Consider elective birth before 37+0 weeks for women with type 1 or type 2 diabetes if there are metabolic or any other maternal or fetal complications.
- Falling insulin requirements in women with pre-existing diabetes is a marker of placental dysfunction and are associated with an increased risk of pre-eclampsia, small-for-gestational age foetuses and still birth
39 weeks
- Advise women with uncomplicated gestational diabetes to give birth no later than 40+6 weeks.
- Consider elective birth before 40+6 weeks for women with gestational diabetes if there are maternal or fetal complications.
- Diabetes should not in itself be considered a contraindication to attempting vaginal birth after a previous caesarean section.
- Explain to pregnant women with diabetes who have an ultrasound‑diagnosed macrosomic fetus about the risks and benefits of vaginal birth, induction of labour and caesarean section
Blood glucose control during labour
- Monitor capillary plasma glucose every hour during labour in women with diabetes, and ensure that it is maintained between 4 and 7mmol/litre
- Intravenous dextrose and insulin infusion should be considered for women with type 1 diabetes from the onset of established labour.
- Use intravenous dextrose and insulin infusion during labour and birth for women with diabetes whose capillary plasma glucose is not maintained between 4 and 7 mmol/litre.
Post-natal care
- Women with insulin‑treated pre‑existing diabetes should reduce their insulin immediately after birth and monitor their blood glucose to establish appropriate dose
- Avoid hypoglycaemia during breast feeding
- Women who have been diagnosed with gestational diabetes should discontinue blood glucose‑lowering therapy immediately after birth.
- Women with pre‑existing type2 diabetes who are breastfeeding can resume or continue to take metformin and glibenclamide
- Women with GDM should be offered fasting glucose between 6-13 weeks or HbA1c after 13 weeks and then annually
Post-natal fasting glucose results
- < 6mmols/litre-Low risk of having diabetes
- 6 – 6.9 mmol/litre-High risk of developing type 2 diabetes
- 7mmol/litre or more-Likely to have type 2 diabetes
References
- NICE guideline: Diabetes in pregnancy: management from preconception to postnatal period. August 2015
