Fibroid (Leiomyoma)
Diabetes in pregnancy
Premenstrual syndrome
Table of content
-
1. Definition
-
2. Incidence
-
3. FIGO Classification
-
4. Complications
-
5. Investigations
-
6. Treatment
-
7. Reference
Fibroid
Definition:
•Fibroids are smooth muscle tumours of the uterus, usually benign but they can have malignant transformations in >1% resulting in leiomyosarcoma
Incidence:
•20-40% of women in reproductive age
•5% to 10% of women presenting with infertility
•Present in 70% of uterus removed at hysterectomy
•Increased incidence in Afro-Caribbean women
•Decreased incidence with prolonged use of combined oral contraceptives
•Decreased incidence with increasing number of term pregnancies
•It has not been identified in pre-pubertal girls and usually shrinks at the time of menopause
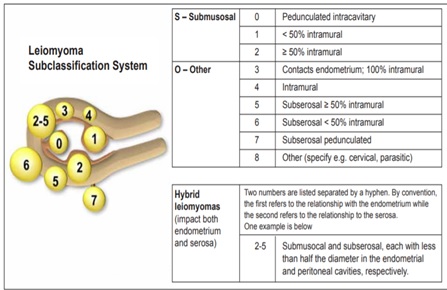
Classification
They are classified as Sub-serosal, Intramural and Submucosal
FIGO Classification
Clinical features
- 50% of fibroids are asymptomatic
- Heavy Menstrual Bleeding
- Anaemia
- Dysmenorrhea
- Dragging and pressure symptoms in the pelvis
- Abdominal swelling
- Urinary frequency and retention
- Bowel problems
- Subfertility-Difficulty in conceiving, pregnancy loss, intrapartum bleeding e.g. during Caesarean section
Complications
- Hyaline degeneration (Painful)
- Red degeneration necrobiosis-occurs during pregnancy due to infarction at mid pregnancy
- Calcification (Womb stone)- usually in postmenopausal women
- Sarcomatous malignant change-0.2% risk, greater risk in women with multiple or rapidly growing fibroid at advanced age
- Infection/abscess-relatively rare
- Torsion of pedunculated fibroid
Investigations
- A large fibroid uterus can often be palpated as a firm pelvic mass.
- The ideal first-line investigation is pelvic ultrasound (transvaginal and transabdominal),
- MRI is useful when planning surgery or as a baseline prior to uterine artery embolisation (UAE)
Treatment
Individualise treatment based on size of fibroid/uterus, fertility desire, patient’s desire to preserve uterus, general medical health, age, Body mass index, previous surgery, previous fibroid treatment, risk and benefit of treatment
Types of treatment
- GnRH agonist
- Selective reversible progesterone modulator
- Levonorgestrel secreting intrauterine system
- Uterine artery embolisation
- Hysteroscopic myomectomy
- Laparoscopic myomectomy
- Abdominal myomectomy
- Hysterectomy
- Uterine artery embolisation
- Magnetic resonance imaging focused ultrasound ablation of uterine fibroid
- Bipolar radiofrequency ablation
Seeking contraception
- 1st step – COC, oral/injected/IUS progestogens, short course of GnRHa
- 2nd step – hysteroscopic myomectomy +/- ablation +/- Mirena IUS. Additional minimally invasive uterus-conserving treatment; UAE, MR focused ultrasonography, laparoscopic uterine artery occlusion and bipolar radiofrequency ablation
- 3rd step – hysterectomy +/- bilateral salpingo-ophrectomy.
Wishing to conceive:
- 1st step – tranexamic acid/NSAIDs
- 2nd step – hysteroscopic myomectomy, laparoscopic myomectomy. Additional minimally invasive uterus-conserving treatments as above
- 3rd step – abdominal myomectomy.
Medical treatment
- GnRH agonist-Causes postmenopausal symptoms and hot flushes. When used prior to myomectomy the plane of cleavage between fibroid and surrounding myomectomy can be masked and make surgery difficult
- Selective progesterone receptor modulator Ulipristal acetate (UPA) shown to be effective in controlling uterine bleeding related to myomas, to reducing myoma size, and to having a good safety profile in the short term.
- UPA is used in a dose of 5mg once daily for up to 3 months for either preoperative or intermittent treatment of moderate to severe symptoms of uterine fibroids in adult women of reproductive age.
Re-treatment should commence only when menstruation has occurred - Levonorgestrel secreting intrauterine system-Relatively contraindicated in distorted cavity. May be expelled during heavy menstruation
- Mefenamic and tranexamic acid can be safely prescribed
Uterine artery embolisation
- Women seeking future pregnancy should not generally be offered uterine artery embolization
- There are lower pregnancy rates, higher miscarriage rates, and more adverse pregnancy outcomes following uterine artery embolization than after myomectomy.
- Studies also suggest that uterine artery embolization is associated with loss of ovarian reserve, especially in older patients.
References
1. StratOG
2. Dewhurst’s Textbook of Obstetrics and Gynaecology
