Epilepsy in pregnancy
Parvovirus infection in pregnancy (Slapped Cheek syndrome)
Terms and Conditions
Epilepsy In Pregnancy
Bank Odusoga DFRSH MRCOG
Table of content
1. Introduction/Incidence
2. Preconception counselling
3. Effects of pregnancy on Epilepsy
4. Effect of epilepsy on fetus
5. When to avoid or postpone pregnancy
6. Management
7. Sudden unexpected death in epilepsy in pregnancy
8. Reference
Introduction/Incidence
- Epilepsy is the most common serious neurological problem encountered in pregnancy affecting 0.5-1.0% of women of childbearing age.
- It is characterised by recurrent, unprovoked seizures resulting from excessive neuronal discharge.
- The risk of mortality for pregnant women is almost 10 times higher than the general population
- Antiepileptic drugs are given in 1 in 200 pregnancies in the United Kingdom
- 2/3rd of women are stable throughout pregnancy
- 96% will deliver a healthy baby
- MBRACE-UK 2015- Highlights need for urgent improvement in the care of pregnant women with epilepsy
- MBRACE ascertained 86% of women with epilepsy who died of Sudden unexpected death in epilepsy had not received pre-pregnancy counselling
Preconception Counselling
- Optimise BMI , reduction of alcohol consumption, advise on smoking cessation, regular exercise
- Remain compliant with Anti Epileptic Drug medication
- Liaise with neurologist to help titrate medication and aim for low dose monotherapy if possible
Reassure Women
- 96% have good outcomes
- Women who are seizure free for > 12 months are likely to remain seizure free if compliant with treatment
Inform
- Some may require dose adjustment to maintain seizure control
- Most can aim for vaginal delivery unless there are obstetric reasons
Effects Of Pregnancy On Epilepsy
- Seizure free 64%
- Increased seizure frequency 17%
- Decreased seizure frequency 16%
- Intrapartum seizure 3.5%
- Status epilepticus <2%
Effect Of Epilepsy On Fetus
Fetus
- Generally low risk to foetus
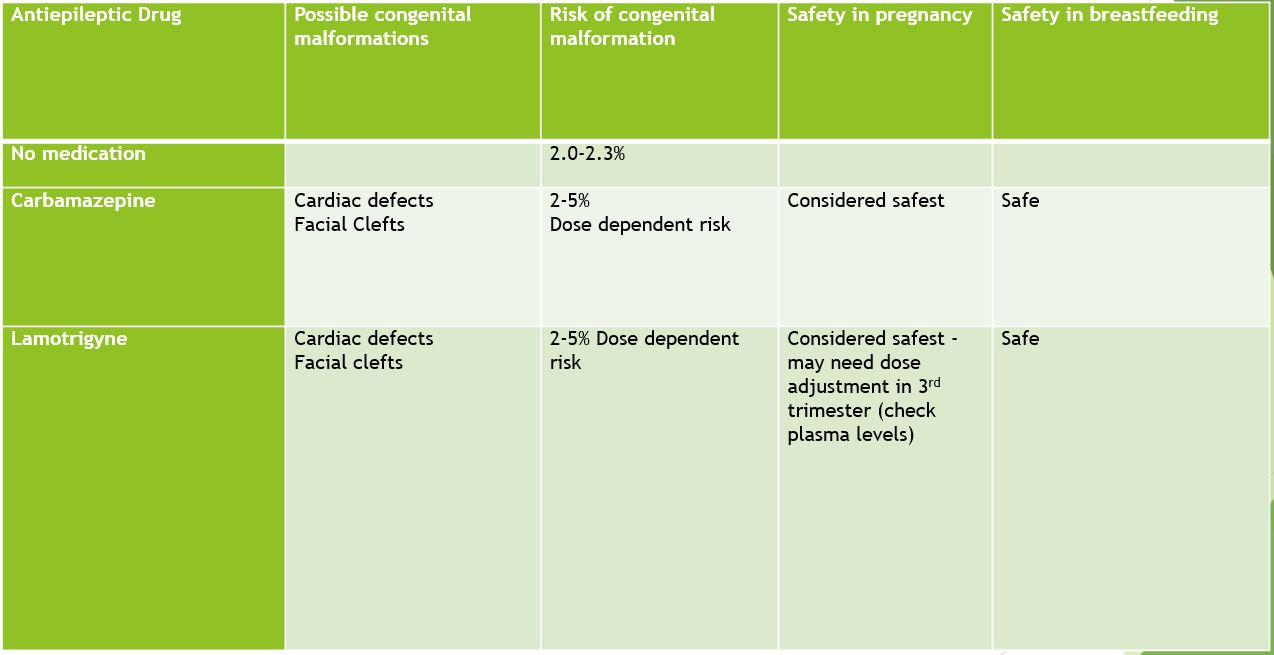
- Increased risks of multiple congenital malformation due to Anti epileptic drugs (Lamotrigine, levetiracetam and carbamazepine are the safest agents)
- Sodium valproate has the highest risk of congenital malformation(neural tube defects, evidence of cognitive difficulties/learning disability)
- Risk of hypoxia and injury from falling during seizures
- Increased risk of growth restriction in those on polytherapy Anti-epileptic drugs
- Risk is dependent on dose and the number of anti-epileptic drugs
- Risk of fetal harm is highest during organogenesis in the 1st trimester
- Risk of cognitive impairment typically occurs in 3rd trimester and is associated with polytherapy
Preconception Medication
- 5mg of Folic acid to be taken several months before and throughout pregnancy this reduces the risk of congenital malformation and cognitive deficits
- Avoid abrupt withdrawal of antiepileptic drugs
- If possible aim for monotherapy with the lowest effective Antiepileptic drug
- If on sodium Valproate consider weaning off or changing to another AED on the advice of a neurologist or Obstetric Physician
- Avoid using sodium valproate as first line in women of child bearing age unless other treatment are ineffective or not tolerated
- If sodium valproate needs to be continued change to moderate release or increase the daily frequency .
- Dose of Sodium Valproate >800mg/day are associated with greater risk of teratogenicity
When To Avoid Or Postpone Pregnancy
- Uncontrolled seizures
- High dose AED
- Polytherapy-Multiple AED
- Drug resistant epilepsy
- Non compliance with medication
- Poor general health
Management
- Unplanned pregnancies should have an urgent review with a neurologist
- Advice women to continue on their AED regimen until a medical review
- In pregnant women presenting with seizures in the second half of pregnancy which can not be clearly attributed to pregnancy manage as eclampsia until a definite diagnosis is made-consider other differential diagnosis e.g. cardiac, metabolic, intracranial conditions and neuropsychiatric conditions including non-epileptic attack disorder
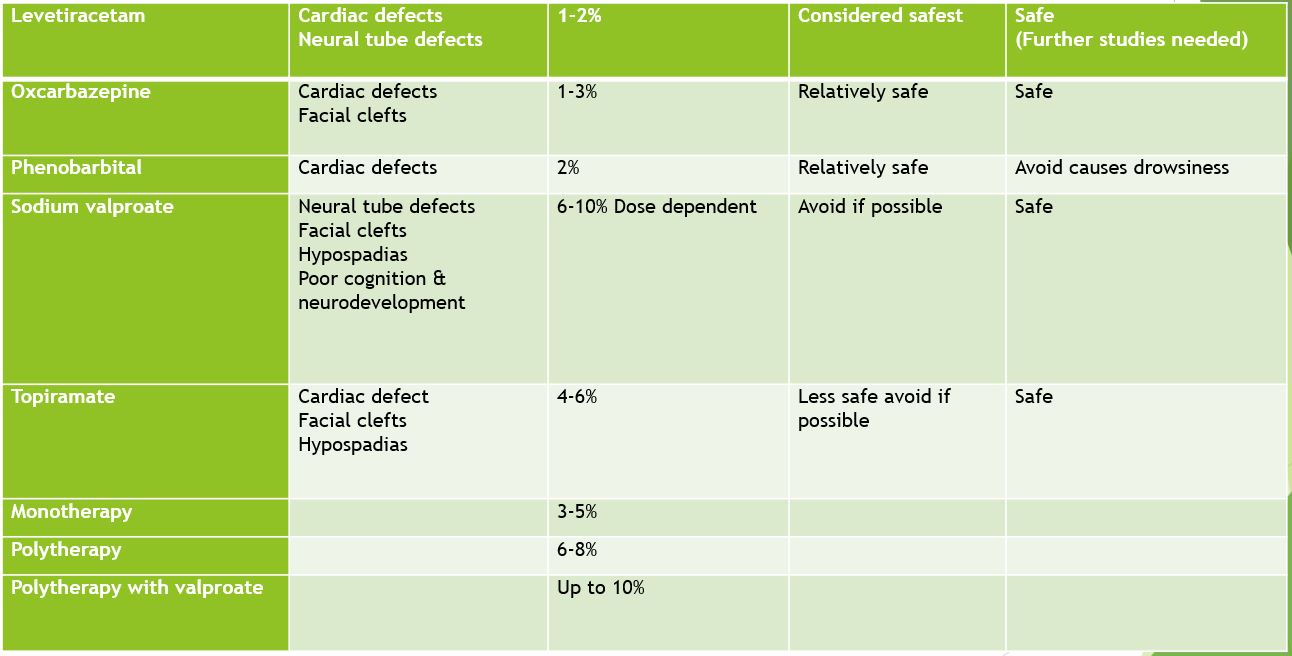
- There may be some women whom the only effective AED is sodium valproate in these circumstances the benefit of valproate for seizure control may outweigh potential risk to fetus. It should only be used after careful discussion with the woman
- Clobazam is also used for exacerbation of seizures during pregnancy or in postnatal period, it is considered relatively safe
Plasma Level Of Antiepileptic Drugs During Pregnancy
- With the exception of lamotrigine, levetiracetam, carbamazepine and oxcarbazepine plasma level monitoring is not required
- Consider monitoring plasma levels of drugs if there is change in seizures frequency, poor compliance and concerns regarding toxicity
Antenatal Care
- Multidisciplinary team: This includes
- Obstetrician with special interest in epilepsy and/or maternal medicine trained
- Neurologist
- Obstetric Physician where available
- General practitioner
- Anaesthetist
- Midwife
- Epilepsy nurse specialist
‘
Take thorough epileptic history at 1st appointment:
Ask following questions and document information
- Who is the neurologist overseeing the care?
- When was epilepsy diagnosed (childhood or teenage onset)?
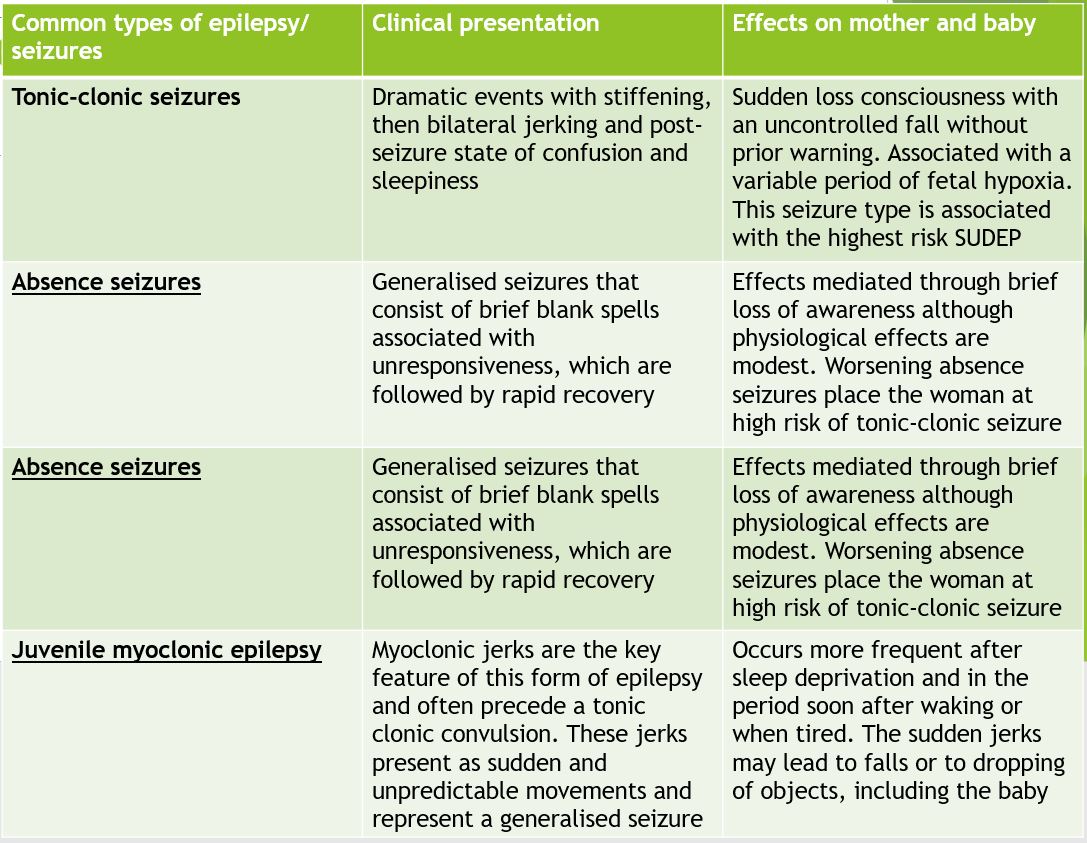
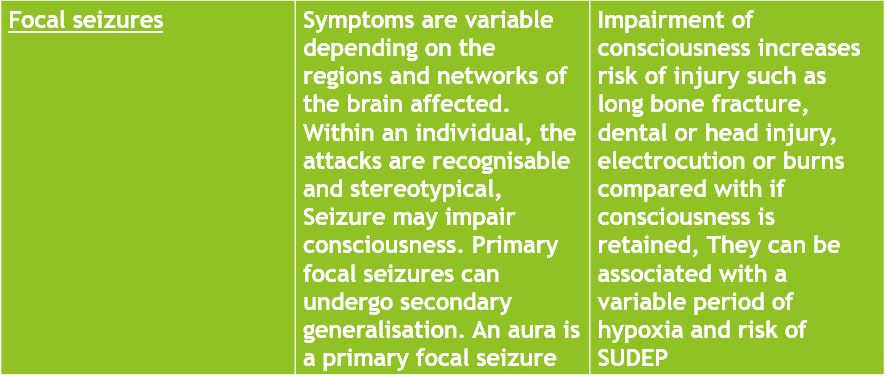
- What type of seizures are experienced? Focal, generalised, non-convulsive or unclassified
- What is the frequency of seizures?
- When was the last seizure?
- What AEDs are taken and at what dose?
- What other features of seizures (triggers, aura, activity during seizure) occur?
- Is there a history of status epilepticus or ITU admission?
Give 5mg of folic acid until at least end of first trimester -RCOG 2016
- There is insufficient evidence for routine maternal vitamin K to prevent haemorrhagic disease of the new born or postpartum hemorrhage
- If there are additional risk factors for Haemolytic disease of the newborn e.g. maternal liver disease or anticipated preterm delivery, consider 10mg oral maternal vitamin K
- Do fetal anomaly scan at 18-20weeks+ 6days to rule out cardiac and neural tube defect
- Do serial growth scan from 28 weeks
- Be alert to signs of depression, anxiety and any neuropsychiatry symptoms in mothers exposed to AEDs
Intrapartum Care
- Reassure women that the risk of intrapartum seizure is low 3.5%
- Delivery should be conducted in a consultant led unit except they have been seizure free for >10 year and not on Antiepileptic drugs for >5years
- Admit in early stages of labour with IV access and one to one midwifery care
- Avoid stress, sleep deprivation, hyperventilation, keep well hydrated and give adequate analgesia
- Continue AEDs in labour
- Clobazam can be considered if there is high risk of seizure in the intrapartum period
- AVOID PETHIDINE-It increases risk of seizures
- Epidural is considered safe
- Well controlled epilepsy per se is not an indication for planned caesarean section or induction of labour
If Seizures Occur In Labour
- Treat with benzodiazepines promptly to reduce maternal and fetal hypoxia and fetal acidosis.(Intravenous lorazepam 2-4mg bolus doses repeated every 10-20minutes or intravenous diazepam 5-10mg slow bolus.
- Nurse in left lateral tilt or manually displace the uterus
- Administer oxygen
- Electronic fetal monitoring should commence
- In refractory cases, intravenous phenytoin can be used
Postnatal Care And Breastfeeding
- All babies born to women taking AEDs should be offered 1mg IM vitamin K to prevent haemorrhagic disease of the new born
- Risk of seizure in the postnatal period is higher than the risk during pregnancy
- Seizures are associated with increase risk of stress, sleep deprivation and reduced drug compliance
- AED dose modified during pregnancy should be reviewed by neurologist and communicated effectively to obstetric team to ensure it is effective in the postnatal period
- There may be a need to reduce dose to avoid toxicity
- Breastfeeding is actively encouraged in the term infant of women with epilepsy
- Caution is advised in women taking polytherapy, phenobarbitone of benzodiazepines or in preterm infants-(they should be monitored closely)
- Advise women to avoid co-bedding and minimise excessive tiredness
- Practical measures include, placing baby in a cot or playpen if mum feels unwell, feeding baby whilst sitting on the floor, changing and bathing baby on the floor, not bathing the baby alone.
- Offer contraception and advice to avoid unplanned pregnancy
- Recommended contraceptive preparations are Levonorgestrel-releasing intrauterine systems, copper coil and medroxyprogesterone injections.
- Women on non-enzyme inducing AEDs (lamotrigine and levetiracetam) can consider estrogen based preparation
- All methods of contraception may be offered to women taking non-enzyme inducing AEDs e.g. sodium valproate, levetiracetam, gapapentin, vigabatrin, tiagabine and pregabalin
- Copper IUD is the preferred choice for emergency contraception.
- Emergency contraception pills with levonorgestrel and ulipristal acetate are affected by enzyme-inducing AEDs
Sudden Unexpected Death In Epilepsy In Pregnancy
- This is death that is unrelated to trauma, drowning or status epilepticus.
- It is the predominant cause of death in women with epilepsy
- AED compliance , first aid training of family members and avoiding sleeping alone may reduce the risk
- SUDEP is higher in women on lamotrigine (2.5 per 1000 patient years) other AEDs (0.5-1.0 per 1000 patient years) this may be due to the relative common usage of lamotrigine and reduced serum drug levels with advancing gestation potentially resulting in increased frequency
