Genital Herpes in Pregnancy
Placenta Praevia and Placenta Accreta
Vulva pain
Genital Herpes in Pregnancy
Dr Funmi Bank Odusoga MRCOG
Table of content
1. Background
2. Classification
3.Incidence
4. Aetiology
5.Transmission
6. Disseminated Herpes infection in mother
7. Management of pregnant women with 1st episode of genital herpes in the 1st and 2nd trimester until 27weeks and 6days
8. Management in the 3rd trimester from 28weeks gestation
9. Management of pregnant women with recurrent herpes
10.Management of women with genital herpes at the onset of labour
11. Genital herpes in preterm pre labour rupture of membranes
12. Management of HIV positive women with HSV infection
13. Management of Neonate
14. Prevention of postnatal infection
15. Reference
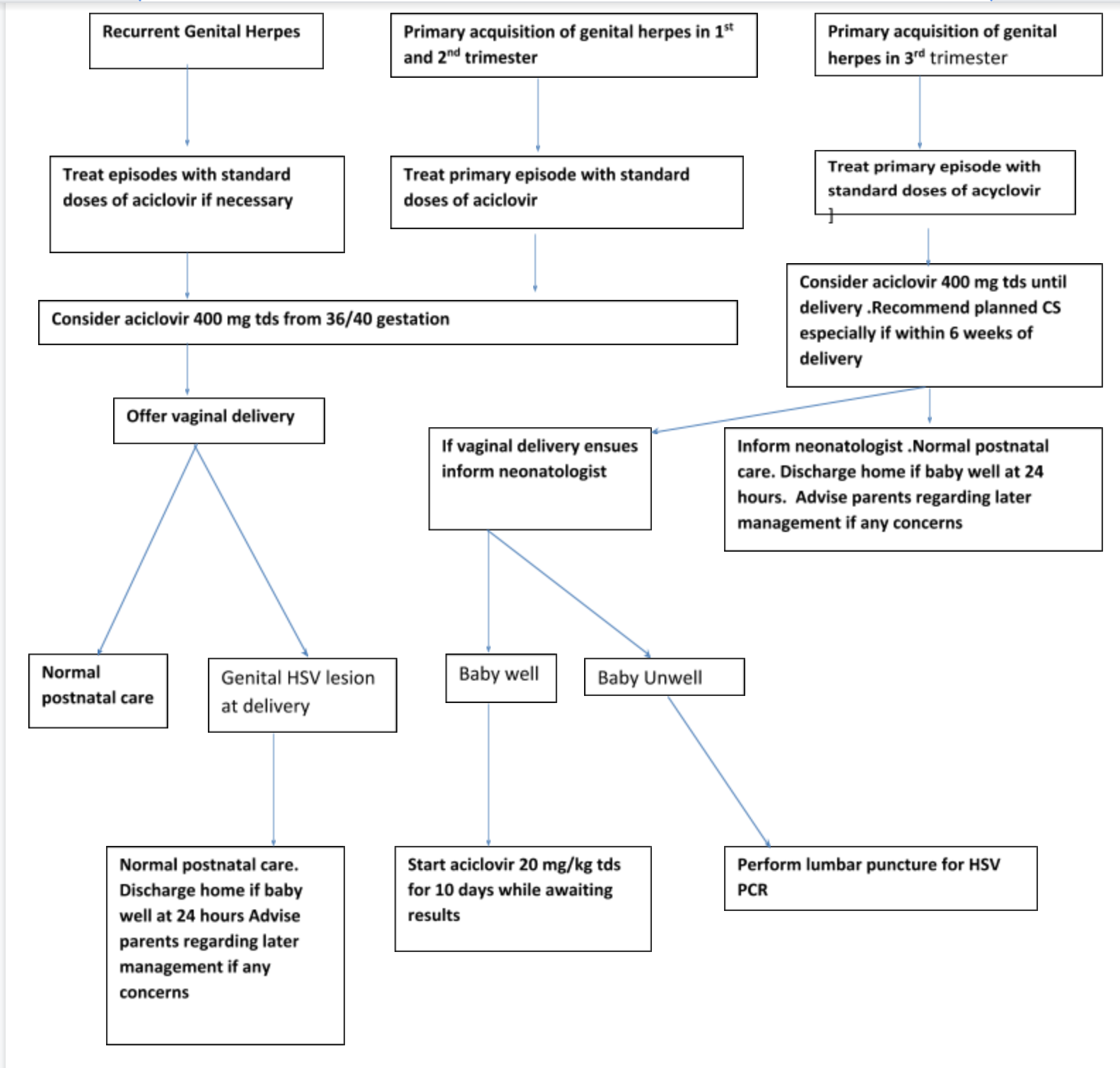
15. Algorithm for the management of herpes in pregnancy and care of neonate
Background
- Neonatal herpes is a very rare but serious viral infection with a high morbidity and mortality.
- Neonatal infection occurs as the result of an infection at the time of birth
- Congenital herpes is extremely rare and occurs by transfer of infection in utero
Classification depending on site
1.Disease localised to skin, eye and/or mouth-
- Represent 30% of Neonatal herpes infection
- With appropriate antiviral treatment, neurological and/or ocular morbidity is less than 2%
2.Local central nervous system (CNS) disease (encephalitis alone)
- 70% of infants with neonatal herpes have disseminated and/or CNS infection
- 60% of infants with local CNS and/or disseminated disease will present without skin, eye and/or mouth infection
- Infants with local CNS disease often present late (generally between 10 days and 4 weeks of age
- With antiviral treatment, mortality from local CNS disease is around 6% and neurological morbidity (which may be lifelong) is 70%
3.Disseminated infection with multiple organ involvement.
- Disseminated disease carries the worst prognosis
- With appropriate antiviral treatment, mortality is around 30% and 17% have long-term neurological sequelae
- The poor outcomes of disseminated and local CNS disease have been attributed to delays between symptom onset and treatment
Incidence of Neonatal herpes
1.65/100 000 live births annually (95% CI 1.3–2.0) UK
1 in 15 000 USA
Aetiology
- Herpes simplex virus type 1 (HSV-1)
- Herpes simplex virus type 2 (HSV-2)
- Approximately 50% of neonatal herpes is due to HSV-1 and 50% due to HSV-2.
- Most cases of neonatal herpes occur as a result of direct contact with infected maternal secretions
- 25% of cases a possible source of postnatal infection was identified, usually a close relative of the mother
- Postnatal infection may occur as a result of exposure to oro-labial herpes infection.
Transmission
- The risks are greatest when a woman acquires a new infection (primary genital herpes) in the third trimester, particularly within 6 weeks of delivery, as viral shedding may persist and the baby is likely to be born before the development of protective maternal antibodies.
- Rarely, congenital herpes may occur as a result of transplacental intrauterine infection. This can lead to fetal growth restriction of fetal death
- Disseminated herpes is more common in preterm infants and occurs almost exclusively as a result of primary infection in the mother
- Recurrent herpes at the time of delivery, which is commonly asymptomatic or unrecognised, may cause the localised forms of neonatal herpes: local CNS disease and skin, eye and mouth infection.
- Transplacentally acquired HSV antibodies do not prevent herpes virus spreading to the brain of the neonate.
- It may be difficult to distinguish clinically between recurrent and primary genital HSV infections, as many first episode HSV infections are not true primary infections.
Risk factors for transmission
- Type of maternal infection (primary or recurrent),
- Presence of transplacental maternal neutralising antibodies,
- Duration of rupture of membranes before delivery
- Use of fetal scalp electrodes and the mode of delivery
Disseminated Herpes infection in mother
- It is rare
- Associated maternal mortality is high
- May present with encephalitis, hepatitis, disseminated skin lesions or a combination of these conditions
- Commoner in immunocompromised women
- Immunocompromised women are at increased risk of more severe and frequent symptomatic recurrent episodes of genital herpes during pregnancy and of asymptomatic shedding of HSV at term
Management of pregnant women with 1st episode of genital herpes in the 1st and 2nd trimester until 27weeks and 6days
- No increased risk of miscarriage in the 1st trimester or association with increased congenital abnormalities
- Refer to Genitourinary medicine physician if genital herpes is suspected for confirmation of diagnosis by Viral polymerase chain reaction, advise on management and screening for other sexually transmitted infections
- Inform Obstetrician
- Administer acyclovir 400mg three times a day for 5days
- Offer paracetamol and topical lidocaine gel for symptomatic relief
- Give intravenous acyclovir if there is disseminated infection
- Acyclovir reduces duration and severity of symptoms and duration of viral shedding
- Though aciclovir is not licensed in pregnancy, there is no evidence of an increased risk of birth defects with aciclovir, famcicloviror valaciclovir if used in the first trimester
- Famciclovir or valaciclovir are not the 1st line recommended in pregnancy as there is less experience with their use in pregnancy
- If delivery does not ensue in the next 6weeks after infection offer vaginal delivery
- Following first or second trimester acquisition, daily suppressive aciclovir 400 mg three times daily from 36 weeks of gestation reduces HSV lesions at term and hence the need for delivery by caesarean section
- Aciclovir administration reduces asymptomatic viral shedding
Management in the 3rd trimester from 28weeks gestation
- There is some evidence of increased perinatal morbidity (preterm labour and low birthweight), together with stillbirth
- There is insufficient evidence to suggest an association between HSV and stillbirth as a cause of fetal death
- In the third trimester, treatment will usually continue with daily suppressive aciclovir 400 mg three times daily until delivery
- Recommend caesarean section as risk of transmission is very high 41%
- It is difficult to differentiate primary and recurrent infection
- 15% of patients presenting with the 1st episode of infection are actually having a recurrent infection
- Type specific HSV antibody testing (immunoglobulin G [IgG] antibodies to HSV-1 and HSV-2) is advisable for women presenting with 1st episode of infection
- The presence of antibodies of the same type as the HSV isolated from genital swabs would confirm this episode to be a recurrence rather than a primary infection and elective caesarean section would not be indicated to prevent neonatal transmission
- May take 2 weeks for the result to be available so manage each case of 1st episode of infection as a primary infection
- Modified delivery care plan if HSV antibody test results subsequently confirm a recurrent, rather than primary infection
- Always discuss results with genitourinary physician or virologist
Management of pregnant women with recurrent herpes
- Inform women that risk of neonatal herpes in low 0-3%
- Majority resolve within 7-10 days without antiviral treatment.
- Offer supportive treatment using saline bathing and analgesia e.g. Paracetamol
- Allow vaginal delivery in the absence of other indication for caesarean section
- Daily suppressive aciclovir 400 mg three times daily should be considered from 36 weeks of gestation (it reduces viral shedding and recurrences at delivery so may reduce the need for caesarean section)
- Polymerase chain reaction culture to identify asymptomatic shedding is not recommended
- There is no increased risk of preterm labour, premature rupture of membranes or fetal growth restriction
- No increased risk of congenital anomalies in women with recurrent genital herpes
Management of women with genital herpes at the onset of labour
Primary episode-management at the onset of labour
- Based on clinical assessment as there is no time for laboratory testing
- Take viral swab as may influence neonatal management
- Inform neonatologist
- Recommend caesarean section in women with primary episode at time of delivery or within 6 weeks of expected date of delivery
- Although benefit of caesarean section reduces after 4hours of ruptured membranes, it is still beneficial to perform caesarean section after this time interval
- Intravenous aciclovir given intrapartum to the mother (5 mg/kg every 8 hours) and subsequently to the neonate (intravenous aciclovir 20 mg/kg every 8 hours) may be considered for those mothers opting for vaginal delivery
- It is unknown whether intrapartum aciclovir reduces the risk of neonatal HSV infection
- Risk of neonatal herpes is 41% if baby is delivered vaginally in patients with primary genital herpes
- Avoid application of fetal scalp electrodes, fetal blood sampling, artificial rupture of membranes and/or instrumental deliveries in women with primary herpes who insist on delivering vaginally
Recurrent Genital herpes-management at the onset of labour
- Inform mother that risk of herpes with vaginal delivery is 0-3%
- Patient should make an informed decision on mode of delivery by considering very low risk of neonatal herpes with vaginal delivery against risk associated with caesarean section
- Given the small background risk (0–3%) of transmission in this group, the increased risk of neonatal herpes infection associated with invasive procedures (e.g. fetal blood sampling, fetal scalp electrode and instrumental delivery) is unlikely to be clinically significant so they may be used if required
- If there is pre-labour rupture of membranes at term, consider expediting delivery to reduce potential exposure of fetus to HSV
Genital herpes in preterm pre labour rupture of membranes (before 37+0 weeks of gestation)
Primary genital Herpes in PPROM
- Discuss with multidisciplinary team , genitourinary medicine, neonatologist and obstetrician
- Decision will be made based on gestational age
- If for immediate delivery then the anticipated benefit of caesarean section remains
- If there is initial conservative management administer IV acyclovir 5mg/kg every 8hours
- Consider prophylactic steroids to reduce the risk of preterm delivery
- If delivery is indicated within 6 weeks of the primary infection, delivery by caesarean section may still offer some benefit despite the prolonged rupture of membranes.
Recurrent genital herpes in PPROM
- When PPROM is encountered in the presence of recurrent genital herpes lesions, the risk of neonatal transmission is very small and may be outweighed by the morbidity and mortality associated with premature delivery.
- Expectant management is appropriate in PPROM before 34weeks
- Offer oral Aciclovir 400mg three times daily for the mother
- After this gestation management is not materially influenced by the presence of recurrent genital herpes lesions
- Administer corticosteroid for fetal lung maturity and to reduce neonatal morbidity and mortality
Management of HIV positive women with HSV infection
Primary HSV Infection
- HIV-positive women with primary genital HSV infection in the last trimester of pregnancy should be managed according to the recommendations for all women with primary genital HSV infection.
Recurrent HSV infection
- Offered daily suppressive aciclovir 400 mg three times daily from 32 weeks of gestation to reduce the risk of transmission of HIV infection, especially in women where a vaginal delivery is planned.
- Mode of delivery should be dependent on obstetric factors and HIV viral load
- There is currently no evidence to recommend daily suppressive treatment of HSV for HIV antibody positive women who are HSV-1 or -2 seropositive but have no history of genital herpes.
Management of the Neonate
Always inform neonatal team in all cases
Born by caesarean section in the 3rd trimester
- Liaise with the neonatal team.
- Swabs from the neonate are not indicated.
- No active treatment is required for the baby.
- Normal postnatal care of the baby is advised with a neonatal examination at 24 hours of age, after which the baby can be discharged from the hospital if well and feeding is established
- Educate parent about good hand hygiene and care to reduce risk of infection
- Advice parent to seek medical help if skin, eye and mucous membrane lesions, lethargy/irritability, poor feeding
Babies born by spontaneous vaginal delivery in mothers with a primary HSV infection within the previous 6 weeks
If baby is well
- Swabs of the skin, conjunctiva, oropharynx and rectum should be sent for herpes simplex PCR.
- A lumbar puncture is not necessary.
- Empirical treatment with intravenous aciclovir (20 mg/kg every 8 hours) should be initiated until evidence of active infection is ruled out.
- Strict infection control procedures should be put in place for both mother and baby.
- Breastfeeding is recommended unless the mother has herpetic lesions around the nipples.
- Parents should be warned to report any early signs of infection such as poor feeding, lethargy, fever or any suspicious lesions
If baby is unwell or presents with skin lesions
- Swabs of the skin, lesions, conjunctiva, oropharynx and rectum should be sent for herpes simplex PCR.
- A lumbar puncture should be performed even if CNS features are not present.
- Intravenous aciclovir (20 mg/kg every 8 hours) should be initiated until evidence of active infection is ruled out.
Babies born to mothers with recurrent HSV infection in pregnancy with or without active lesions at delivery
- Conservative management of the neonate is advised.
- Liaise with the neonatal team.
- Surface swabs from the neonate are not indicated.
- No active treatment is advised for the baby.
- Normal postnatal care of the baby is advised with a neonatal examination at 24 hours of age, after which the baby can be discharged from the hospital if well and feeding is established.
- Educated parent regarding good hand hygiene and due care to reduce risk of postnatal infection.
- Parents should be advised to seek medical help if they have concerns regarding their baby. In particular, they should be advised to look for: skin, eye and mucous membrane lesions, lethargy/irritability, and poor feeding.
If clinical evidence of poor feeding and sepsis
- Surface swabs and blood for HSV culture and PCR.
- Intravenous aciclovir (20 mg/kg every 8 hours) should be given while awaiting cultures.
- Further management by the neonatal team according to condition of the baby and test results.
Prevention of postnatal infection
-
- In 25% of cases a possible source of postnatal infection is responsible, usually a close relative of the mother
- Efforts to prevent postnatal transmission of HSV are therefore important and advice should be given to the mother regarding this.
- The mother and all those with herpetic lesions who may be in contact with the neonate, including staff, should practice careful hand hygiene.
- Those with oral herpetic lesions (cold sores) should not kiss the neonate.
References
- Summary of RCOG/BASHH guideline Management of Genital herpes in pregnancy
Algorithm for the management of herpes in pregnancy and care of neonate