Pelvic Organ Prolapse
Acute management of thromboembolism disease in pregnancy and puerperium
Cervical insufficiency/cerclage
Pelvic Organ Prolapse
by Dr Ilze Zommere
Table of content
1. Definition
2. Incidence and Epidemiology
3. Risk factors
4. Comorbidities
5. Symptoms
6. Examination
7. Classification and grading
8. Other investigations
9. Prevention
10. Non-Surgical management
11. Surgical management
12. Complications of surgery
13. References
Definition
- Falling, slipping or downward displacement of the uterus and/or the different vaginal compartments and their neighbouring organs such as bladder, rectum or bowel.The International Urogynecological Association (IUGA) and International Continence Society (ICS)
Incidence and Epidemiology
- Difficult to estimate its prevalence and incidence accurately
- 9% of women overall report symptoms of prolapse
- 31-40% of women would have a degree of pelvic organ prolapse, depending on the method of examination as well as the background features of women examined
- The lifetime risk of undergoing prolapse surgery ranges from 11% to 19%
Risk Factors
- Age – age is associated with levator ani muscle fibrosis, even in nulliparous patients
- Pregnancy – incidence of 50% in parous compared to 2% in nulliparous women + Vaginal delivery is associated with levator ani muscle fibrosis as well as pudendal neuropathy and thus more risk of pelvic organ prolapse than caesarean section ( but NNTT analysis revealed that 7 women need to have C/S to avoid 1 POP)
- Tears/episiotomy at delivery increase risk of POP
- Instrumental delivery and birth weight – evidence of this is conflicting
Demographic risk factors
- Ethnicity – hispanic American women > white American women > African American women
- Obesity
- Smoking
- Occupation – jobs that involve heavy lifting, such as nursing, manual work and housework, have been shown to be significantly associated with vaginal prolapse (housewives POP > in comparison to managerial/professional women; odds ratio 3.1, 95% confidence interval 1.6–8.8 )
Comorbidities
- Chronic constipation – chronic straining for defecation not only increases intra-abdominal pressure but can cause pelvic floor muscle denervation from pudendal nerve stretch with perineal descent
- COPD – chronic pulmonary disease is associated with increased risk of pelvic floor repair after hysterectomy
- Oestrogen deficiency and HRT
- Family history and genetic risk
- Connective tissue disease – joint hypermobility syndrome , varicose veins and rectal prolapse, h/o hernia
Symptoms
- Vaginal bulge, or lump down below
- Bearing down sensation
- Backache
- Vaginal bleeding
- Stress incontinence of urine
- Frequency of micturition and urgency as well as urge incontinence ( OAB)
- Voiding dysfunction, retention, double voiding
- Recurrent UTIs
- Obstructed defecation
- Rectal frequency and urgency
- Anal incontinence
- Dyspareunia/apareunia
Support to the uterus
- The cardinal ligaments hold the cervix, and upper vagina, in place
- The uterosacral ligaments hold the back of the cervix, and upper vagina, in place and help, alongside the round ligaments, maintaining the anteversion flexion position of the uterus
Examination
- Describe the maximum protrusion noted by the individual during her daily activities
- Describe inspection findings – atrophy, ulceration, leakage of urine on cough, other
- Demonstrate the prolapse on examination, including on standing and straining ( Valsalva), or applying traction on the prolapse
- Confirm with patient that the protrusion seen by you is most severe protrusion what she has experienced
Classification
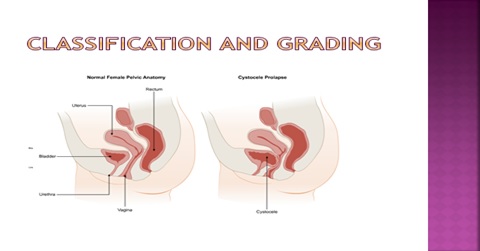
Anterior compartment
- Cystocele
- Urethrocele
- Cystourethrocele
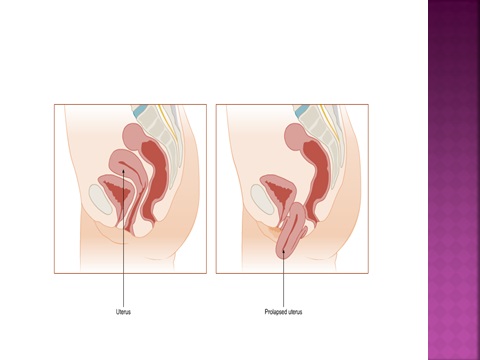
Apical Compartment
- Uterine
- Uterovaginal prolapse
- Post hysterectomy vaginal vault prolapse
- Enterocele
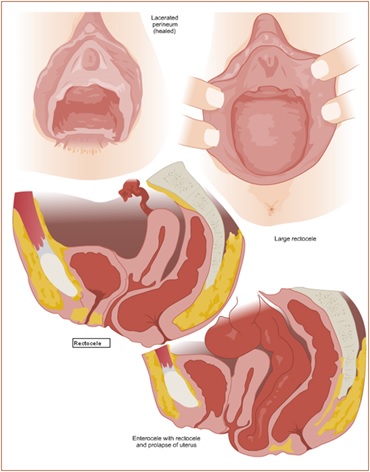
Posterior compartment
- Rectocele
- Enterorectocele
Grading of POP
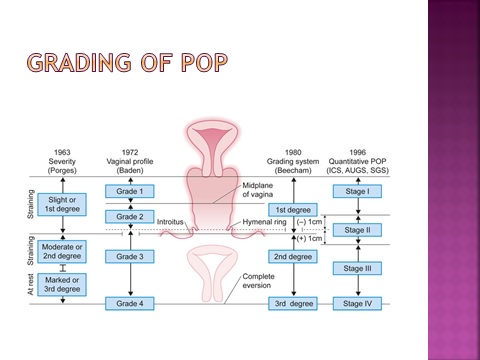
Definition of landmarks
- Hymen – preferable to introitus- defined as plane ‘0’
- The anatomic position of the six defined points for measurement should be
- Centimetres above or proximal to the hymen (negative number)
- Centimetres below or distal to the hymen (positive number
The pelvic organ prolapse quantification POP-Q system
- Based on measuring the distance between two specific points for each compartment in addition to the length of the vagina, genital hiatus as well as the perineal body. The 6 points are:
- point Aa – 3 cm proximal to the external urethral meatus
- point Ba – most distal part of the anterior vaginal wall
- point C – most distal part of the cervix, or vaginal vault
- point D – the posterior fornix, in those who still have their cervix
- point Ap – 3 cm proximal to the hymen, on the posterior vaginal wall
- point Bp – most distal part of the posterior vaginal wall
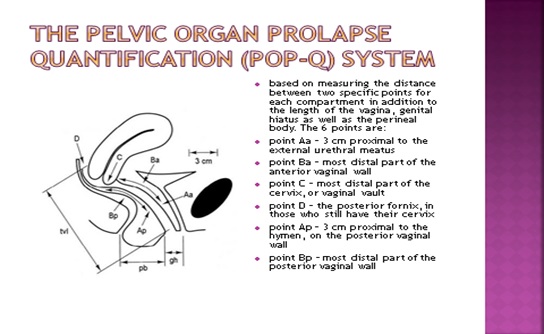
Recording of examination findings in centimetres
| Anterior wall – Aa | Anterior wall – Ba | Cervix or Cuff – C |
| Genital hiatus – GH | Perineal body – PB | Total vaginal length – TVL |
| Posterior wall – Ap | Posterior wall – Bp | Posterior fornix – D |
Pelvic organ prolapse staging
- Stage 0 – No prolapse, points Aa, Ap, Ba and Bp are –3 and point C is between –TVL and –TVL–2
- Stage 1 – Most distal point <-1 (more than 1 cm above the hymen)
- Stage 2 – Most distal point ≥ –1 and ≤1 (between 1 cm above and 1 cm below the hymen)
- Stage 3 – Most distal point > 1 but < TVL-2 (more than 1 cm below the hymen, but at least 2 cm less than the total vaginal length)
- Stage 4 – Most distal point > TVL –2 (complete vaginal eversion, with <2 cm of the vaginal wall still above the hymen).
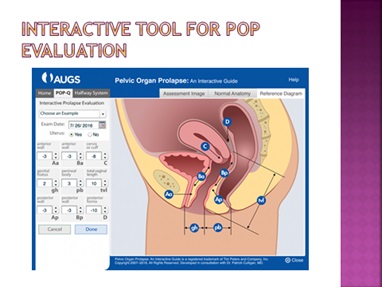
Interactive tool for POP evaluation
Other investigations
- Urine testing for infection
- Urodynamics
- Radiological investigations -Defecography (defecatory proctography/evacuation proctography)
- MRI
- Ultrasound
Prevention
- Avoiding anything that may increase intraabdominal pressure – excess weight, chronic chest conditions, constipation, heavy lifting
- Pelvic floor protection-preventing severe perineal tears, physio therapy timely
- Surgical techniques at hysterectomy – to obliterate POD
Non-Surgical management
Pessary
Choice of pessary depends on a number of factors:
- age of the woman
- sexual activity
- previous hysterectomy
- menstrual history
- extent and type of prolapse
- previous pessary use and outcome
- ease of attendance for pessary replacement
Judging the pessary size and type comes with experience and is a matter of trial and error
- The vagina must be free of ulceration and this should be confirmed during prolapse assessment (treatment is local oestrogen cream or pessary for 2-3 weeks)
- After insertion – women should be asked to walk for few minutes, go to the toilet and try to pass urine
- The frequency of replacement varies from 3 to 6 months
Problems with pessary use
- Difficult removal and insertion
- Neglected pessary
- Vaginal ulceration
- Bleeding ( due to ulceration, fistula, malignancy)
- Vaginal discharge
- Pain and constipation
- Change of size and/or type of pessary
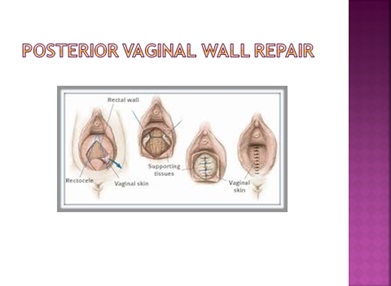
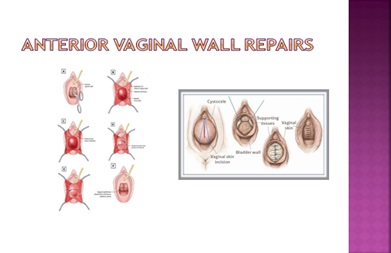
Surgical management
Choice will depend on the same factors, including:
- nature of symptoms and degree of bother
- nature and extent of prolapse
- completion of family and future pregnancy plans
- sexual activity
- age
- fitness for surgery and anaesthesia
- associated incontinence symptoms
- the woman’s goals
- work, physical activity and domestic circumstances
- previous management and outcome
- surgical experience and familiarity with different surgical procedures
- having realistic expectations about outcomes, in the light of history and examination
Surgical treatment
- Route – vaginally, abdominally or laparoscopically with or without hysterectomy
- Recurrence of prolapse of failure of procedure is up to 29%
Postoperative care importance
- vaginal pack and indwelling catheter inserted for 6 to 24 hrs
- Bladder care – post voiding residual urine after catheter removal
- Advice – heavy lifting, strenuous exercises, prolonged straining etc. should be avoided for 3 months. Sex can be resumed about 6 weeks after surgery.
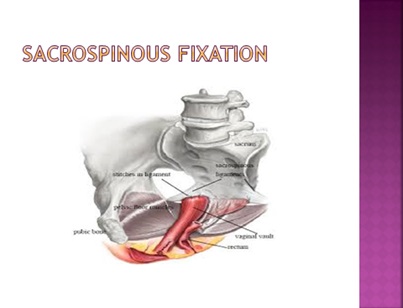
Uterine preservation procedures
- Sacrospinous hysteropexy
- Manchester repair/fothergill’s repair
- Sacrohysteropexy
- Laparoscopic uterosacral ligament plication
Complications of surgery
- Bleeding
- Bladder, ureter or bowel injury: if not detected and repaired at the time can lead to urinary / bowel fistula
- Infection: either wound or urinary tract infection
- Initial voiding dysfunction may be encountered
- Failure and recurrence of prolapse
- Dyspareunia is usually the result of tight vaginal repair. Women may try lubrication and vaginal dilators first though some may require Fenton’s repair
- Conversion to laparotomy may be required for bleeding or visceral injury that cannot be managed vaginally
References
Stratog on line resource
