Acute Uterine Inversion
Management Of Ectopic Pregnancy
Intrahepatic Cholestasis of Pregnancy / Obstetric Cholestasis
Table of content
-
1. Introduction
-
2. Incidence
-
3. Definition
-
4. Classification
-
5. Risk factors
-
6. Diagnosis
-
7. Examination
-
8. Management
-
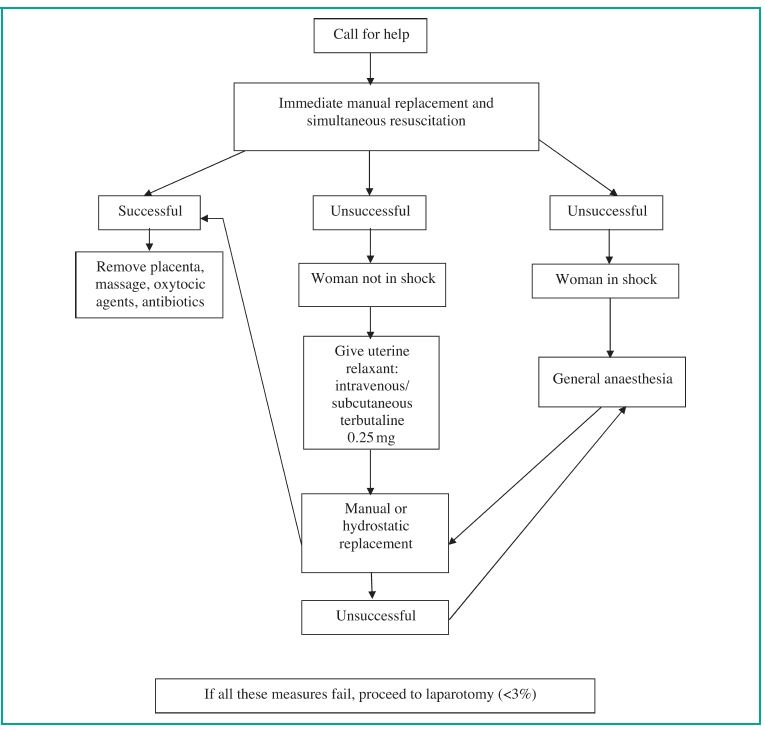
9. Flow chart
-
10. Reference
Acute Uterine Inversion
Dr ‘Funmi Odusoga MRCOG (Consultant O&G)

Introduction
- Described by Hippocrates. (460-377BC)
- Soranus of Ephesus AD110
- Ambroise-Pare- 16th century
Incidence – Varies
- Depends on geographical location
- 3times higher in India than USA
- 1:3737
- Four fold decrease in incidence of acute uterine inversion associated with vaginal birth after the introduction of active management of the 3rd stage-from 1in 2304 to 1 in 10044
Definition
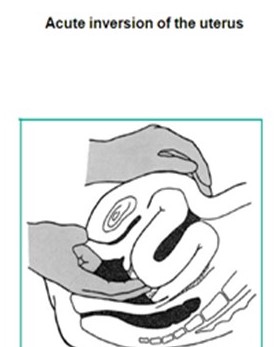
- Acute uterine inversion occurs when the uterine fundus collapses into the endometrial cavity turning the uterus completely or partially inside out.
- It is a rare complication of vaginal delivery and a life threatening Obstetric emergency.
Classification – Classified by the extent of inversion
- 1st degree – (Incomplete) inversion: the fundus is within the endometrial cavity
- 2nd degree – (Complete) inversion: the fundus protrudes through the cervical os
- 3rd degree inversion (Uterine Prolapse): the fundus protrudes to or beyond the introitus
- 4th degree – (total uterine and vaginal) inversion: both the uterus and vagina are inverted
Risk Factors
- 50% have no risk factors
- Management of the 3rd stage-either by excessive cord traction or at manual removal
- Fundal placenta with a short umbilical cord
- Uterine atony
- Fundal implantation of morbidly adherent placenta
- Placenta praevia
- Manual removal of placenta
- Connective tissue disorders e.g. Ehlers – Danlos syndrome, Marfan’s syndrome
Pathophysiology
Three possible events
- A portion of uterine wall prolapses through the dilated cervix or indents forward
- Relaxation of part of the uterine wall
- Simultaneous downward traction of the fundus leading to inversion of the fundus
Diagnosis is based on clinical findings
- The vast majority present with haemorrhage with or without shock, abdominal pain and the presence of a smooth round mass protruding from the cervix or vagina
- Patient may also present with signs of circulatory shock in the absence of visible or recorded blood loss. This shock is neurogenic in origin. Patients in neurogenic shock present with bradycardia (low pulse rate) and hypotension (low blood pressure) but with time, postpartum haemorrhage will ensue.
- A high index of suspicion is required where shock is out of proportion to blood loss. This can help in making an early diagnosis and avoid haemorrhage.
Examination
- On abdominal examination the uterine fundus is absent at its expected periumbilical position. On vaginal examination the inverted fundus fills the vagina
- If the uterus is only partly inverted the diagnosis may not be obvious except on vaginal examination
- Complete inversion is an easier diagnosis, as the fundus of a completely inverted uterus will be visible at the introitus
Management:
- The key to a successful outcome is teamwork, resuscitation and repositioning of the uterus
- If you Suspect diagnosis:
- Call for help alerting the Obstetric emergency team ( Senior Obstetrician, Anaesthetist, Midwife, porters to send and retrieve crossmatched blood)
- Attempt immediate manual replacement and resuscitate the patient simultaneously by inserting 2 wide bore cannulas and retrieving blood for FBC, Cross-matching (6units of blood), Electrolytes, urea and baseline clotting. Administer adequate IV fluid to support blood pressure. Institute post- partum haemorrhage management
- Please note: Delay can render replacement progressively more difficult and increase the risk of haemorrhage
- If placenta is still attached please DO NOT remove it until the uterus is replaced
- If manual replacement is unsuccessful in theatre, hydrostatic replacement (O’Sullivan technique) should be used.
Hydrostatic Method
- Exclude uterine rupture
- With the woman in lithotomy, rapidly instil sterile water or isotonic sodium chloride into the vagina via a rubber tube or intravenous giving set
- Bag of fluid should be elevated approximately 100-150cm above the level of the vagina. You may require up to 4-5 litres of fluid
- Maintain a tight seal on the introitus with your hand or with a silastic ventouse cup if necessary
- The fluid distends and pushes the fundus upwards into its natural position by hydrostatic pressure
- Should the above technique fail then laparotomy should be considered
Laparotomy
Huntingdon’s Operation
The abdomen is opened and the inversion site is exposed. A crater will be noted in the region of the cervix, with indrawn tubes and round ligaments. Two Allis forceps are introduced into the crater on each side and gentle upward traction is exerted on the forceps, with a further placement of forceps on the advancing fundus. By doing this, the uterus is pulled out of the constriction ring and restored to its normal position
Haultain’s Operation
In this operation the cervical ring is incised posteriorly with a longitudinal incision. The rest of the steps are similar to Huntingdon’s method. Once the uterus has been repositioned all incisions in the cervix, uterus and vagina are closed with interrupted sutures. Uterotonics are given to maintain contraction of the uterus.
Recent Techniques
Vijayaraghvan et al-.26 reported a case where acute inversion of the uterus was managed under laparoscopic guidance, citing the advantages of laparoscopic surgery as the reason for the procedure. Consideration, however, needs to be given to the woman’s haemodynamic status and the possible effects of pneumoperitoneum.
Antonelli et al.-41 reported a case where laparotomy was performed and a silastic cup used from above for the correction of complete acute inversion of the uterus. The stated advantages of using a silastic cup were that it was gentler on the tissues and afforded easy placement and manoeuvring through the constriction ring.
Management After Correction Of Inversion
- Commence 40unit of Syntocinon infusion in 500mls of Saline at 125mls/hr and other haemostatic agents as required. Refer to guidelines for Management of post partum haemorrhage
- Manage on delivery suite for 24hrs post partum
- Debrief the woman about the events surrounding acute uterine inversion
- Reassure patient that fertility and reproductive outcomes are not compromised
Inform patient about risk of recurrence and the need for hospital delivery in subsequent pregnancies
Flow chart