Chronic Pelvic Pain
Premenstrual syndrome
Thyroid disease in pregnancy
Table of content
1. Definition & Epidemiology
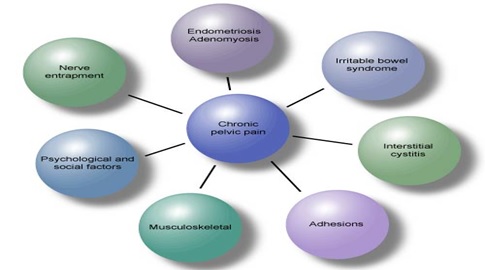
2. Aetiology & Contributory factors
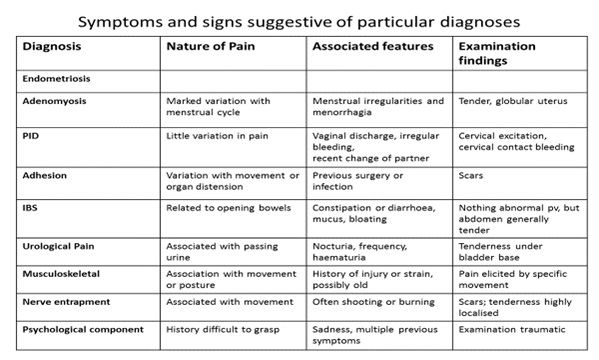
3. Symptoms and signs suggestive of particular diagnosis
4. Red flag symptoms
5. Assessment-History, Examination and Investigations
6. Treatment
7. Reference
Definition
-
- Pain is defined by IASP as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in those terms.
- CPP is defined as intermittent or constant pain of at least 6months duration felt in the lower abdomen or pelvis, not associated exclusively with menstruation, intercourse, pregnancy or malignancy
- It is a symptom and not a diagnosis
Epidemiology
- CPP is common, a large community survey in the UK-3months prevalence 16.9% (similar results in the U.S and New Zealand
- In general practice women present with CPP as commonly as they complain of asthma and migraine
- 50% of patient in the community and 28% in primary care have no diagnosis.
Cyclical variation in pain
- The severity of symptoms of many non-gynaecological disorders are known to vary across the menstrual cycle. These include irritable bowel syndrome, interstitial cystitis, fibromyalgia, rheumatoid arthritis and migraine. Though this may be an effect of hormonal changes on the disease pathology, a number of studies have shown cyclical variations in pain thresholds and tolerance which may account at least in part for these symptoms and their response to (or aggravation by) hormonal treatments. Cyclical variation in the inputs from the uterus, ovaries or endometrial deposits may also be relevant.
Aetiology & Contributory factors
Adenomyosis
- The presence of heterotopic endometrial glands and stroma in the myometrium with adjacent smooth muscle hyperplasia”. It can be diffuse disease or be localised to form an adenomyoma.
- Occurs in 1% of women, coexists with 12% of endometriosis.
- Clinical presentation: Menorrhagia, dysmenorrhea, irregular bleeding, dyspareunia, CPP, subfertility
Chronic PID and Adhesions
- Adhesions may be a cause of pain particularly on organ distension and stretching. Dense vascular adhesions may cause CPP.
- Adhesion may be caused by endometriosis, previous surgery or previous infection.
- Two recognised distinct from of adhesive ovarian disease are
- Residual ovary syndrome: A small amount of ovarian tissue inadvertently left behind following oophorectomy which may become buried in adhesions.
- Trapped ovary syndrome: A retained ovary becomes buried in dense adhesion post hysterectomy.
Irritable Bowel Syndrome
- Irritable bowel syndrome: Affects approx. 20% of adult female population
- It may be associated with dyspareunia and there may be cyclical variation in symptoms.
- Diagnosis is clinical and all features may not be present
Rome III criteria for the diagnosis of IBS
- Continuous or recurrent abdominal pain or discomfort on at least 3 days a month in the last 3months, with the onset at least 6 months previously, associated with at least 2 of the following
- Improvement with defecation
- Onset associated with a change in frequency of stool
- Onset associated with a change in the form of stool
Interstitial cystitis
- It is a chronic inflammatory disorder of the bladder.
- Pathophysiology remain elusive, it is a spectrum of painful bladder syndrome.
NIDDK initial criteria (1987)
- Automatic diagnosis: Hunner’s ulcer
- Positive factors (two needed):
- Pain on filling, relieved by emptying
- Suprapubic, pelvic, vaginal or perineal pain
- Glomerulations on endoscopy
- Decreased cystometric compliance
NIDDK revised criteria (1988)
- Presence of bladder pain or urinary urgency
- Glomerulations or Hunner’s ulcer
Exclusions:
- Cystometric (awake) capacity 350 ml
° Using fill rate 30–100 ml/minute, absence of intense
urge to void at 100 ml gas or 150 ml liquid
- Involuntary contractions on cystometry
- Awake frequency 8/day
- No nocturia
- Duration 9 months
- Age 18 years
- Cystitis (bacterial, chemical, tuberculosis, radiotherapy)
- Prostatitis, vaginitis
- Bladder, uterine, cervical, vaginal or urethral cancer
- Active herpes
- Bladder or lower ureteral calculi
- Urethral diverticulum
Musculoskeletal pain
- May be a primary source of pelvic pain or an additional component resulting from postural changes.
Nerve entrapment
- In scar tissue, fascia or a narrow foramen may result in pain and dysfunction in the distribution of that nerve entrapment
- It is defined as highly localised sharp, stabbing or aching pain, exacerbated by particular movements, and persisting beyond 5weeks or occurring after a pain free
- The incidence of nerve entrapment after one pfannesteil incision is 3.7%
Psychological and social
- Depression & sleep disorders are common (consequence rather than a cause of pain)
- Complex relationship with physical and sexual abuse Child sexual abuse may initiate a cascade of events or reactions which may make an individual more vulnerable to
Red flag symptoms
- Bleeding per rectum
- New bowel symptoms over 50years of age
- New pain after the menopause
- Pelvic mass
- Suicidal ideation
- Excessive weight loss
- Irregular vaginal bleeding over 40years of age
- Post coital bleeding
Assessment-History, examination and Investigation
History
- Discuss multifactorial nature of Chronic pelvic pain from the start. The aim should be to develop a partnership between the clinician and the woman to plan a management programme.
- Adequate time should be allowed for initial assessment
- Women should feel they have told their story and that they have been listened
- Allow women to discuss the theory, ideas or a concern about the origin of the pain.
- Encourage women about their symptoms and ideas
- Ask about pattern of pain and its associations with urinary, bowel, psycho-social and its effects on movement and posture.
- Complete pain diary for 2-3 menstrual cycle. (To identify provoking factors & temporary associations)
- Red Flag symptoms should be identified and managed appropriately
- Refer non-gynaecological pain to appropriate specialty e.g gastroenterology, genitourinary medicine, physiotherapy, psychosexual counsellor
Examination
- Abdominal and pelvic exam, look for focal tenderness, enlargement, distortion, tethering, or prolapse. (revelation of new information).
Investigations
- Screening for Sexually transmitted Infection.
- Positive endocervical sample supports but does not prove the diagnosis of PID,
- Negative result for Chlamydia and gonococcus does not rule out PID.
- Transvaginal scan –appropriate investigation to identify and assess adnexal masses. Little predictive value for the assessment of other causes of CPP including endometriosis
- Transvaginal and Magnetic Resonance Imaging are useful to diagnose Adenomyosis
- Role of MRI in diagnosing small deposit of endometriosis is uncertain.
Diagnostic Laparoscopy:
- It is the Gold standard for investigation.
- Better seen as 2nd line investigation if other therapeutic investigations fail. Risk of death 1 in10,000 and risk of visceral injury 2.4 in 1000 of whom 2/3 will require laparotomy
- 33-50% of laparoscopies will be negative and much of the pathology identified is not necessarily the cause of pain.
- Serum Ca125 should be done if persistent or frequently (>12times per month)-bloating, early satiety, pelvic pain or urinary urgency or frequency.
- New IBS symptom in women over 50years of age should prompt serum Ca125 measurement
Treatment
- If no Gynaecology element in history refer to appropriate specialty
- Use symptom diary
- If the pain is cyclical, a diagnostic trial with Combined oral contraceptive pill, Gonadotropin releasing hormone analogues, levonorgestrel-Intrauterine device for 3-6 months should be offered before diagnostic laparoscopy
- Offer Analgesia if no other therapeutic intervention is to be initiated yet.
- Refer to pain management if pain not adequately controlled
- Try adjuvant treatment amitriptyline or Gabapentin for neuropathic pain
- Transcutaneous nerve stimulation, acupuncture and other complimentary therapies may be useful for some women.
- Laparoscopic uterosacral nerve ablation is ineffective in the management of chronic pelvic pain.
- Treat any condition found at laparoscopy e.g. endometriosis, adhesions, ovarian cyst, Fimbriae cyst etc. Treatment of findings at laparoscopy may not relieve symptoms
- IBS-Offer women a trial with antispasmodics
- Encourage amendment in diet to attempt to control symptoms.
- Adhesion-Division of dense adhesion should be considered as this is associated with pain relief.
- No evidence to support the division of fine adhesions in women with CPP
Reference
RCOG green top guideline No 41 published 2012
