Endometriosis
Thyroid disease in pregnancy
Thalassemia in Pregnancy
Endometriosis

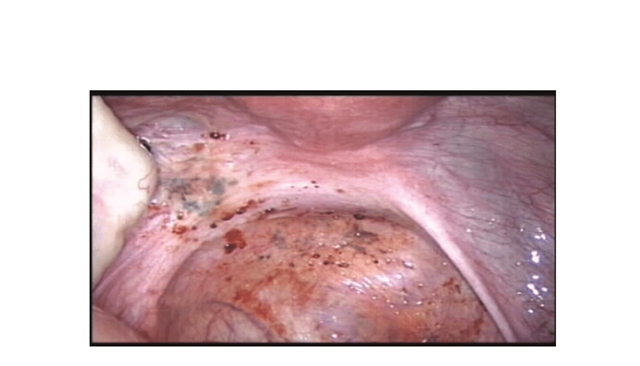
Table of content
-
Definition
-
Incidence
-
Prevalence-Diagnostic delays
-
Clinical presentations
-
Diagnosis
-
Management
-
Management Algorithm
-
References
Definition
-
-
- Endometriosis is defined as a pathologic condition in which the endometrium, consisting of endometrial glands and stroma, is found in locations outside the endometrial cavity and uterine musculature
- Usual location is the Pelvis
- Extra pelvic sites: including anterior abdominal wall, surgical scars, diaphragm, omentum, small intestine, appendix, lung, urinary tract, musculoskeletal, and neural systems.
-
Incidence
-
-
- Varies 10-20% of reproductive age women
- True prevalence is not known because gold standard diagnosis requires a laparoscopy
- 5% in patients with chronic pelvic pain
- 6%-50% in patients with infertility
- 1% in patients having tubal ligation
- Women with endometriosis are 3.5times likely to have received a diagnosis of IBS when compared with controls
-
Diagnostic delays
Several studies have reported large diagnostic delays in endometriosis
On average 8years in the UK
Causes of delays suggested
-
-
- Intermittent use of contraceptives causing hormonal suppression of symptoms
- Use of non-discriminatory examination
- Misdiagnosis
- Attitude towards menstruation and normalization of pain by the women, their mothers, family doctors, gynaecologists and other specialist
-
Many women report that their delay in diagnosis leads to increase personal suffering, prolonged ill health and a disease state that is more difficult to treat
Aetiology -Remains Unknown
-
-
- Hypothesis
- Retrograde menstruation
- Altered immune environment
-
Clinical presentation
The combination and severity of symptoms correlates poorly with the extent of disease found at laparoscopy
-
-
- Could be asymptomatic
- Dysmenorrhoea
- Chronic Pelvic pain
- Dysparenuia
- Infertility
- Ovulation pain (Mittelschmerz)
- Dyschezia (Pain opening the bowels)
- Cyclical bowel or bladder symptoms
- Chronic fatigue and malaise
-
Examination
-
-
- Findings associated with endometriosis include:
- Fixed, retroverted uterus
- Tender/nodular uterosacral ligaments
- Visible nodules on the cervix/vagina
- Palpable rectal nodules
- Enlarged/tender ovaries
-
Above signs may be more obvious if the woman is examined during menstruation. However, this is unacceptable to many women
Diagnosis
-
-
- Gold standard-Laparoscopy and histology of visible lesions. Negative diagnosis does not exclude it.
- If ovarian endometrioma of >3cm histology should be obtained to exclude malignancy
- Transvaginal/rectal USS-To exclude endometrioma of nodules in bladder and rectum
- MRI- to exclude deep infiltrating and uterosacral disease and adenomyosis
-
Management
Medical Management
-
-
- Nonsteroidal anti-inflammatory drugs (NSAIDs) and other simple analgesia
- Combined oral contraceptive pill (COCP) –can try back to back for 3months
- Danazol (200-800mg daily for 3-6months) has androgenic side effect and voice deepening may be irreversible
- Gestrinone- (androgen derivative of 19 nortestosterone)
- Progestogens, e.g. medroxyprogesterone acetate
- GNRH analogue -add HRT if using longer than 6months to maintain bone mass
- Mirena (LNG-IUS).
- Treat symptoms empirically without laparoscopic diagnosis
- Hormonal treatments suppress rather than cures and needs repeating because of symptom recurrence
-
Surgical management
-
-
- It is effective with reports of reduction in pain score, improvement in quality of life, sexual function.
- Ablation/Excision/ Total Laparoscopic Hysterectomy and Bilateral salpingo-ophrectomy
- Ablation for endometriomas results in lower recurrence rates, lower infection rates and higher spontaneous pregnancy rates
- Deeply infiltrating disease should be managed at a specialist unit where all disease can be excised. A pelvic MRI should be performed before surgery and careful preoperative discussion is essential, including information about the risk of bowel perforation, fistula formation and ureteric damage. As an adjunct to surgery for deep endometriosis, 3 months of gonadotrophin-releasing hormone agonists should be considered prior to operating.
- Consider TLH/BSO and excision of all visible endometriosis if family is completed. Offer HRT till age 50-51-consider combined HRT rather than oestrogen only to avoid the theoretical risk of recurrence and malignant transformation
-
Adjuvant medical treatment
-
-
- Consider 3 months administration of GNRH analogue before surgical management of deep infiltrating endometriosis involving bowel, ureter and bladder
- Offer Mirena or COCP after surgical management to reduce recurrence after surgical treatment
- Aromatase inhibitors- can be considered in patient with rectovaginal disease that is refractory to other treatments (there are concerns with mineral bone density)
-
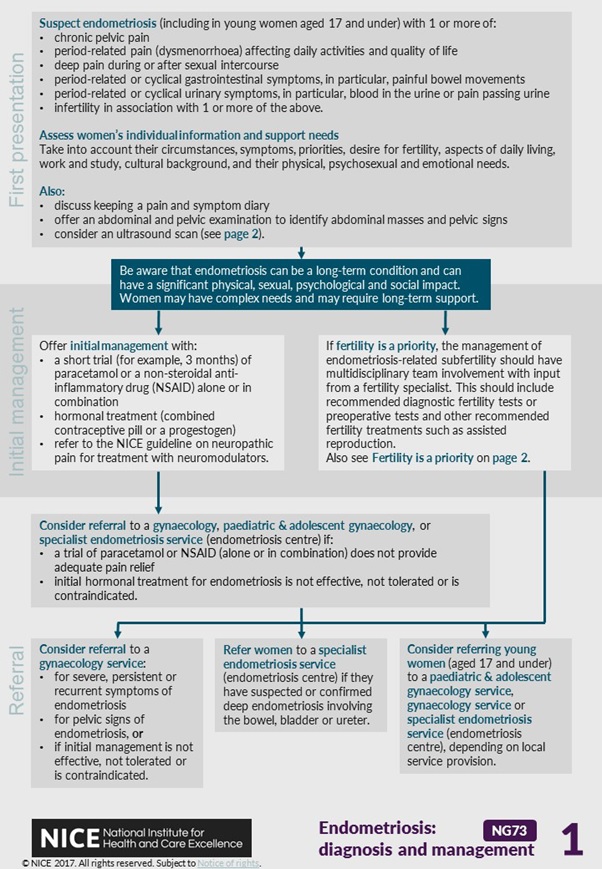
Management Algorithm
References
-
-
- Endometriosis and management: NICE guideline [NG73] Published date: September 2017
- StratOg
-
