Infertility
Terms and Conditions
Massive Obstetric Haemorrhage
Infertility
Miss Nikoletta Panagiotopoulou MRCOG MSc MD Consultant in Reproductive Medicine
Table of content
1. Definition
2. Epidemiology
3. Factors affecting the Chance of Conception
4. Pre-conceptual advice
5. Major causes of subfertility
6. Management options
7. Legal issues
8. Essential points for general practitioners
9. References
Definition
- Primary subfertility – Delay in conception for a couple who have no previous pregnancies
- Secondary subfertility – Delay in conception for a couple who have conceived previously, even if pregnancy did not end with a successful outcome (e.g. Miscarriage, ectopic)
Epidemiology
- 15% of couples experience subfertility
- 50% of them will conceive spontaneously or with simple advice/ treatment
- 8% of the population remain sub-fertile & require complex treatment
- 50% of them will have 1ry subfertility
- 50% of them will have 2ndary subfertility
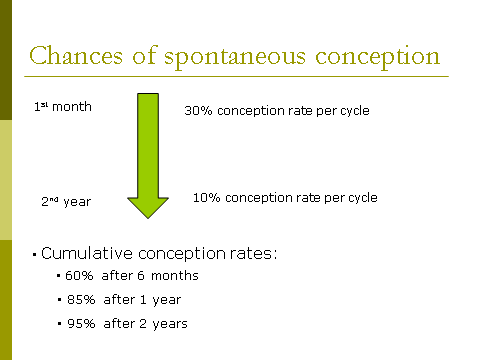
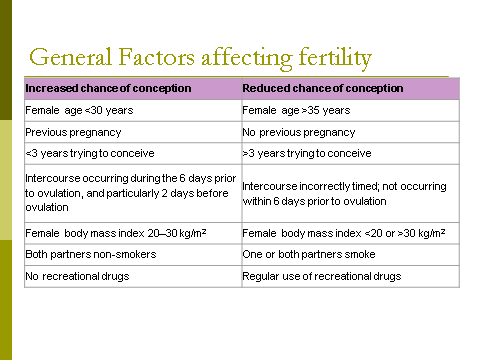
Factors Affecting The Chance Of Conception
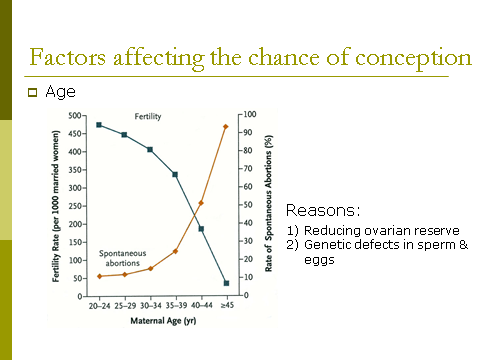
- Age
- Previous pregnancy
- Duration of subfertility
- Timing of intercourse during the menstrual cycle
- Extremes of body mass index
- Others
Previous pregnancies
- Couples with secondary subfertility have higher chance of conception in relationship to couples that never conceived before
Duration of subfertility
- If the duration of subfertility is less than 3yrs,a couple is more likely to conceive than couples who have been trying for longer
Timing of intercourse – The probability of conception…
- Rises from 6 days before ovulation
- Peaks 2 days before ovulation
- Falls markedly by the day of ovulation
Dunson Study
Extremes of BMI
- Pregnancy is less likely for women with BMI > 30kg/m2 or < 20kg/m2
Other Factors – Smoking, Caffeine, Alcohol, Recreational drugs, Anabolic steroids
Pre-conceptual advice
| Factors | Advice/Action |
| Pre-existing medical problems |
· Stabilise medical conditions and ensure medical control is optimal · Check if drugs used are safe for use in pregnancy/do not have impact on sperm function · It may be appropriate to refer a woman with a significant medical problem to an obstetric physician for advice about implications of the condition in pregnancy |
| Weight |
· Check BMI · Advice regarding weight gain or loss as appropriate if BMI <20 kg/m2 or >30 kg/m2 |
| Smoking | · Advise both partners to stop smoking |
| Recreational drugs | · Advise both partners to stop using recreational drugs |
| Timing of intercourse |
· Check understanding of menstrual cycle and relate most fertile days to the length of female partner’s cycle (from 6 days before ovulation up to the day of ovulation; peak chance is at 2 days before ovulation) · Intercourse occurring regularly 2–3 times a week should cover the most fertile time |
| Folic acid |
· All women who are trying to conceive should take folic acid supplements (0.4 mg) daily to reduce the risk of neural tube defects (Neural tube defect) · Folic acid 5 mg daily for women with history of previous Neural tube defect, epilepsy or other relevant medical comorbidities |
| Virology screening |
· Screen for rubella serology and offer immunisation to those not immune · Consider screening for HIV, and hepatitis B and C in high risk groups |
Major causes of subfertility
| Major causes of subfertility | Percentage |
| Ovulation disorders | 20 – 30% |
| Tubal damage | 20 – 30% |
| Male factor | 25 – 40% |
| Unexplained | 10 – 20% |
| Endometriosis | 5 – 10% |
| Other problems, e.g. fibroids | 4% |
Investigations
Factors warranting early investigation
| Factors in female | Factors in male |
|
Age > 35 years Previous ectopic pregnancy Known tubal disease or history of PID / STD Tubal or pelvic surgery Amenorrhoea or oligomenorrhoea Evidence of a psychosexual problem |
Testicular maldescent / orchidopexy Chemotherapy or radiotherapy Previous urogenital surgery History of STD Varicocele Erectile or ejaculatory disorder |
Investigations continued
| Who | Test | When | Why |
| Female with regular cycle | Anti-Mullerian Hormone/ Antral follicle count | Anytime | Assess ovarian reserve |
| Female with regular cycle | Progesterone |
Mid-luteal phase (adjust to cycle length minus 7 days prior to expected menses) Do on day 21 for 28 day cycle and day 28 for 35 day cycle |
Assess ovulation |
| Female – irregular cycle or amenorrhoea |
FSH, LH, Estrogen, Prolactin, TSH, FT4, Testosterone, Serum Hormone Binding Globulin, Free Androgen Index, 17-OH-Progesterone |
Early follicular phase |
Assess pituitary and underlying ovarian function Establish cause of oligomenorrhoea / amenorrhoea |
| Female – all |
Rubella serology Cervical smear Transvaginal ultrasound scan |
Ø Any time Ø If due Ø Anytime |
Ø Confirm immunity Ø Ensure up to date Ø Assess pelvic anatomy, ovarian reserve |
| Male – all | Semen analysis | Sample after 2–5 days abstinence. If first sample is abnormal, consider perform a second sample after 3 months or sooner if indicated | Assess sperm production |
To check for tubal damage do either
- Hysterosalpingogram (HSG)
- Hysterocontrastsonography (HyCoSy) or
- Laparoscopy & dye test- if previous PID, known endometriosis or inconclusive HSG or HyCoSy
Management Options
- Ovulation Induction
- Intrauterine Insemination – IUI
- In-vitro fertilisation – IVF +/- Intra-cytoplasmic sperm injection (ICSI)
- Donation-Sperm, eggs, embryos
- Commence treatment as soon as a diagnosis is made
- Allow 2 years of trying in patient with unexplained sub-fertility before commencing treatment if age is not an issue
Ovulation Induction
Indication –
- Patient with anovulation,
- Consider in unexplained infertility
Methods of ovulation induction
- Anti-oestrogen-Clomiphene 50mg day 2-6 of period, Tamoxifen
- Gonadotrophins-FSH and LH
- Ovarian drilling
Side effects of ovulation induction
- Multiple pregnancy
- Ovarian hyperstimulation syndrome
- Theoretical risk of ovarian cancer if there is prolonged usage
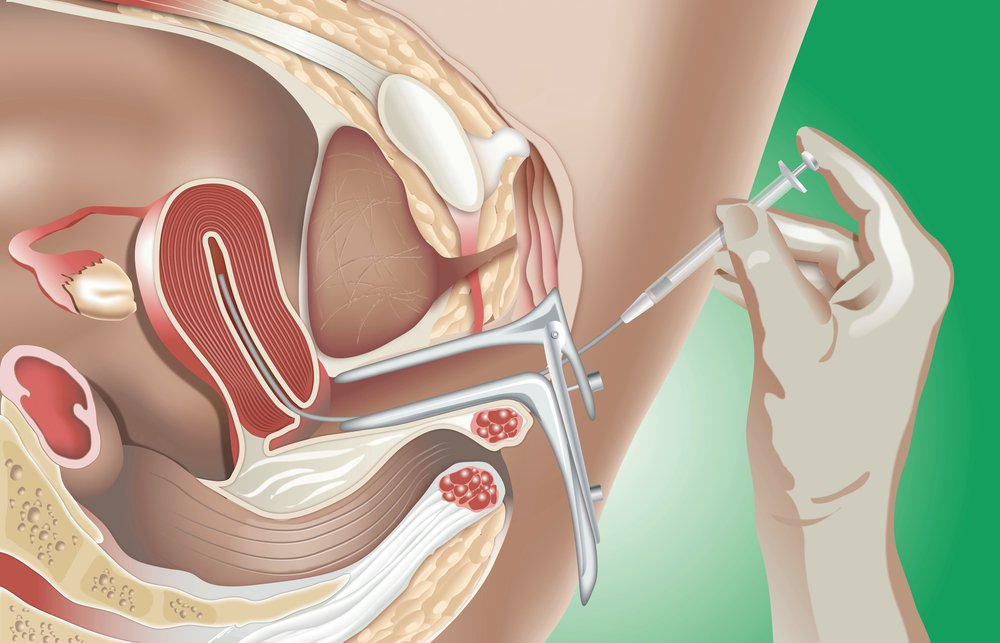
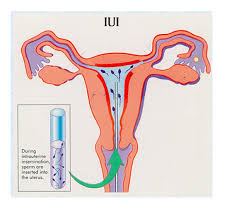
Intrauterine Insemination
Indication
- Unexplained infertility
- Inability to have sexual intercourse
- It can be combined with ovulation induction or done in a natural cycle
Sperm are inserted into the uterus during artificial insemination
Invitro Fertilization / Intracytoplasmic Sperm Injection
Indication
- Tubal Infertility
- Male factor +/- ICSI
- Ovulation disorders
- Unexplained infertility
- Failure of other treatments
Method
Step 1 – Oocyte collection
- Transvaginal ultrasound guided approach
- GA or conscious sedation
- hCG or Buserelin (depending on stimulation protocol) is given 36-37 hrs prior to O.C. to induce the final oocyte maturation step
- Procedure lasts 15 mins
- Average of oocytes = 10 ( aiming for 5 -15)
Then
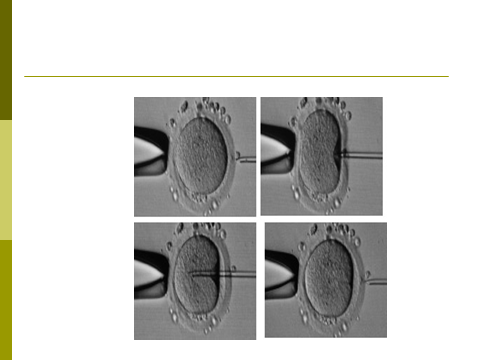
Step 2 -Fertilization
- Natural
- C.S.I.
- ICSI indications: Severe defects in semen quality, Previous poor/failed fertilisation
Then
Step 3 Embryo transfer
- How many embryos?
- Risk of multiple pregnancy
- After embryo transfer luteal phase supported with progesterone
- May be able to freeze ‘spare’ embryos
Success rate
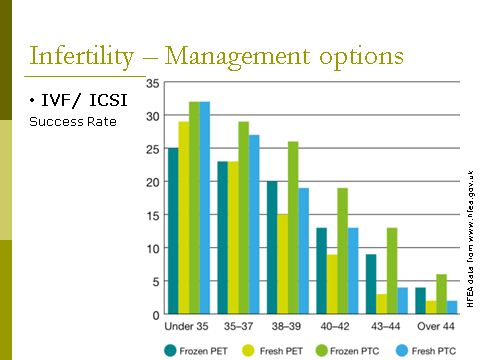
- Y axis is percentage
- X axis is age range
(PET) Birth rate per embryo transferred- The number of births divided by the sum of embryos transferred for treatment embryo transferred (PET) cycles starting in that year
(PTC) Birth rate per treatment cycle-The percentage of treatment cycles started in that year which resulted in a live birth.
Legal Issues
Human Fertilization & Embryology Act
It covers:
- creation & use of human embryos outside the human body
- use of human embryos in research
- use of donated gametes & embryos
- provision about people with a parental responsibility
- Regulates ART activities via its licensing & inspection processes
Essential point for General Practitioners
The most important role for the GP in managing individuals or couples with fertility problems is that of advocacy ensuring that couples receive the correct advice, investigations, management and referral.
NICE recommends that couples, who have failed to conceive after one year of unprotected intercourse are offered further clinical assessment and investigation (2). However, earlier assessment should be offered where the woman is 36 years or more or if there are known causes of infertility.
You should refer a person to a fertility specialist if they have the following:
No success after 12 months of unprotected sex for women aged under 36, and six months for women over 36,
A diagnosis of PCOS,
Irregular cycles,
Endometriosis or a history suggestive of tubal damage,
Recurrent miscarriage (two or more consecutive pregnancy losses),
Premature menopause,
Poor semen quality,
Genetic conditions such as Turner syndrome, cystic fibrosis, Klinefelter syndrome etc.
The initial assessment and investigation in primary care is aimed at evaluating the main causes of infertility. Generally speaking, the causes of infertility may be expressed as sperm problems, tubal problems, ovulation disorders and unexplained infertility. Prevalence of each cause varies from study to study, but is approximately 25% for each. The vast majority of women with an ovulatory disorder will have polycystic ovary syndrome (PCOS) and many women with PCOS are overweight or obese.
Initial assessment of the infertile individual or couple should include a detailed medical history. In obtaining individuals’ medical history, special emphasis should be given on the following:
- Female menstrual history. This will help determine the likelihood of ovulation dysfunction
- Medical co-morbidities. Medical co-morbidities that affect female fertility include: hypo/hyperthyroidism, prolactinoma, PCOS, hypothalamic pituitary disease, eating disorders, Cushing’s disease and premature ovarian failure. In addition, medical co-morbidities can adversely affect male fertility
- Conditions that are linked with high risk of tubal damage, such as abdominal operations, sexually transmitted infections, a history of pelvic inflammatory disease and endometriosis
- Medications use. Male and female fertility can be affected by certain drugs, such as sulphasalazine, nitrofurantoin, tetracyclines, cimetidine, ketoconazole, colchicine, allopurinol, alpha-adrenoceptor-blocking agents, propranolol, chemotherapeutic alkylating agents, cannabis, cocaine and anabolic steroids
- Smoking, alcohol and drug use, as these can have a detrimental effect upon fertility and pregnancy.
- Coital history to ensure frequent unprotected intercourse.
Clinical examination should focus on identifying weight problems for either partner, as well as feature of PCOS, thyroid problems or Cushing’s disease for the female partner. Assessing female BMI is important particularly in relation to PCOS and obesity or amenorrhoea and anorexia. A high or very low BMI may also restrict access to some complex treatments. A pelvic examination for the female partner is usually not necessary. However, it is good clinical practice to record the female BP as it also provides a pre-pregnancy baseline.
Fertility investigations that can be performed in general practice are aimed at
identifying the cause(s) of infertility described above.
Assessment of male factor:
Semen analysis should be performed on behalf of all couples presenting with infertility where a male partner is present. If the first sample is abnormal a second sample should be taken 3 months later.
Assessment of tubal status:
For the assessment of tubal damage, women who are not known to have co-morbidities (such as PID, previous ectopic pregnancy or endometriosis) should be offered hysterosalpingo-contrast-sonography (HyCoSy) or hysterosalpingography. Women with co-morbidities should be offered laparoscopy and dye as other pelvic pathology can be assessed at the same time.
Before uterine instrumentation is done, women should be offered chlamydia trachomatis and gonorrhoea screening and treatment where necessary.
Assessment of ovulation:
For women with regular menstrual periods, confirm ovulation with mid- luteal (Day 21 of a 28-day cycle) progesterone. Depending on the duration of the menstrual cycle, this test may need to be conducted later in the cycle (e.g. Day 28 of a 35 – day cycle).
For women with irregular periods, serum FSH, LH and oestradiol should be measured in the early follicular phase. High FSH and low oestradiol implies premature ovarian failure. Low FSH, LH and oestradiol implies hypothalamic/pituitary disease.
Additional investigations:
- Offer thyroid function tests to women with symptoms of thyroid disease or oligo/amenorrhoea
- Offer serum prolactin test to women who have oligo/amenorrhoea, galactorrhoea or a pituitary tumour.
- Offer serum testosterone and SHBG (sex hormone binding globulin) to women with oligo/amenorrhoea to assist with the diagnosis of PCOS.
- Offer 17aOH Progesterone to women with high serum testosterone to exclude congenital adrenal hyperplasia.
- Offer pelvic ultrasound scan to assist with the diagnosis of PCOS and assess the uterus and ovarian reserve.
- Offer serum anti-mullerian hormone (AMH) test to assess ovarian reserve
Management strategies for primary care include offering general advice, obesity management and may also include ovulation induction for a small cohort of infertile couples.
Couples should be advised to
- have regular UPSI every 2 – 3 days,
- limit the use of alcohol, and
- stop smoking.
In addition, men should be advised to avoid tight fitting underwear and avoid testicular hyperthermia.
Women should be advised to lose weight, if their body mass index is greater than 29 kg/m2, and to take 400 mcg folic acid before conception and up to 12 weeks of pregnancy. Women on anticonvulsants, or with diabetes, or with a history of a child with a neural tube defect should be offered 5 mg folic acid per day.
Watchful waiting is appropriate for women aged less than 36 years and where no cause for infertility has been identified following initial investigations described above. Following initial assessment couples with male factor or tubal infertility should be referred to specialist units that can deliver IVF/ICSI treatments.
Reference:
- Wilkes S, Chinn DJ, Murdoch A et al. Epidemiology and management of infertility. Fam Pract 2009; 26: 269-74.
- NICE. Fertility problems: assessment and treatment. CG156. London, NICE, 2015
Quiz
- On average, 20% of couples in the general population will conceive within one year if they do not use contraception and have regular sexual intercourse
- On average, 20% of couples in the UK will experience fertility problems
- Women trying for a pregnancy should be advised to have sexual intercourse to coincide with ovulation.
- Smoking is unlikely to have an effect on female fertility.
- Men with a body mass index of more than 30 are likely to have reduced fertility.
- What are the factors affecting a couple’s chance of conceiving?
- Which of these factors cannot be aided by fertility treatment?
- What factors may affect tubal function?
- Which factors may have an effect on sperm production
- Most couples presenting with failure to conceive are infertile.
- Over 80% of couples less than 35 years of age will conceive within 12 months of trying for a pregnancy with regular sexual intercourse.
- Female age is more important than male age when considering chances of conception.
- After 3 years of unexplained subfertility a couple still have a >10% chance of conceiving per menstrual cycle.
- Obesity is an independent risk factor in female subfertility.
Answers
- False
- True
- False
- False
- True
- female age, ovulation, sperm production, fallopian tubal function, uterine function, duration of trying, lifestyle factors, e.g. obesity and smoking, medical history, previous pregnancy
- female age, duration of trying, previous pregnancy, (uterine function)
- Infection – chlamydia, gonorrhoea, pelvic inflammatory disease ,pelvic surgery, endometriosis
- Male obesity, Smoking, Alcohol, Body building drugs
- False
- True
- True
- False
- True
Reference
