Intrahepatic Cholestasis of Pregnancy / Obstetric Cholestasis
Acute Uterine Inversion
Management of breech presentation
Intrahepatic Cholestasis of Pregnancy / Obstetric Cholestasis
Caroline Finch MSc/ Dr Odusoga MRCOG
Table of content
1. Definition
2. Incidence
3. Causes
4. Risk
5. Clinical Features
6. Diagnosis of Obstetric Cholestasis
7. Investigations
8. Management
9. Essential points for general practitioners
10. Reference
Definition
- Obstetric cholestasis is a multifactorial condition of pregnancy characterised by pruritus in the absence of a skin rash with abnormal liver function tests (LFTs), neither of which has an alternative cause and both of which resolve after birth
Reference: Royal College of Obstetricians & Gynaecologists. (2011) Green-top Guideline No. 43. Obstetric
Cholestasis
- When the normal flow of bile out of the liver is reduced. Chemicals in the bile called bile salts (also often referred to as bile acids) can then build up and ‘leak’ into the bloodstream. This causes affected women to have increased levels of bile salts in their blood.
Incidence
- Prevalence in European countries is about 0.5% – 1%
- 1 in 140 pregnancies in UK
- Women of Indian and Pakistani descent seem to have a higher risk
- Is the most common pregnancy related-specific cause of hepatic impairment
Causes of Obstetric Cholestasis
Genetic
- Positive family history – found in about 35% of patients/ 12% of patients sisters are affected
Hormonal
- Pregnancy causes an in increase in oestrogen and progesterone hormones,these can affect the liver in a way which slows down the rate of bile passing out along the tiny bile ducts. Some pregnant women may be more sensitive to these hormonal effects.
Risk
Fetal Risk
- Intrapartum fetal distress – 12% – 22%
- Meconium liquor 25% – 45%
- Spontaneous pre term delivery 12% – 44%
- Intrauterine fetal death
- Fetal intracranial haemorrhage
- Fetal risk maybe related to maternal bile acids levels
- Fetal complications increased by 1% – 2% per additional 1µmol/L over 40µmol/L of serum bile acids
- A UK prospective study of bile acids >40µmol/L demonstrated that risks of preterm delivery and meconium stained liquor rose with increasing serum bile acids
Maternal Risk
- Vitamin K deficiency due to malabsorption of fat-soluble vitamins
- Possible increased risk of PPH
Clinical feature
- Severe pruritus affecting the limbs and trunk – particularly the palms and soles.
- Pruritus worse at night
- Developing in the second half of pregnancy – usually during the third trimester (80% present after 30 weeks) probably because hormone levels is at peak
- Associated with insomnia and malaise
- There may be excoriations – NO RASH
- associated with dark urine, anorexia
- Pale stools
Diagnosis of Obstetric Cholestasis
Diagnosis of exclusion made in 3 steps
- Typical history of pruritus without rash
- Abnormal LFT’s/Bile acids
- Exclusion of other causes of itching and abnormal liver function
Investigations
- Serum bile acids levels are the most sensitive and specific biochemical marker
- Elevated levels of alanine transaminase (ALT) and aspartate transaminase (AST) are supportive of the diagnosis
- Increase in alkaline phosphatase is usually placental in origin and does not normally reflect liver disease
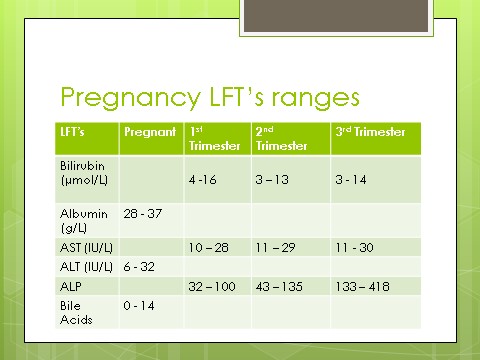
- Pregnancy specific reference ranges for LFTs should be used
- Liver scan
- Coagulation screen (PT, APTT and INR) – due to malabsorption of Vitamin K
- Immunoglobulin levels
Management
Antenatal
- Consultant led care
- Follow up in Antenatal day unit weekly –
- LFT’s and bile acids weekly
- Report any RFM
- CTG and USS for growth if patient reports reduced fetal movement
- Follow up every 2 weeks in ANC
- Consider delivery by 37+6 weeks if raised serum bile acids
- If serum bile acids >/= 40µmol/L – closer monitoring is indicated
- Ursodeoxychloic Acid – improves pruritus, transaminases and bile acids in most women with ICP – 80-90% (Nelson-Piercy 2015)
- Dose 500mgs BD and increased in increments of 500mgs every week if no response – total daily dose of 2 grams
- Mechanism of action of ursodeoxycholic acid: May protect the hepatocyte membrane from the damaging toxicity of bile salts and enhance bile acid clearance across the placenta from the fetus
- Vitamin K 10mgs daily if prothrombin time is prolonged or INR >1.3
- Antihistamines -Piriton or Promethazine may help relieve pruritus
- Topical emollients-Diprobase, calamine lotion and aqueous cream with menthol – safe in pregnancy and clinical experience suggest they may provide slight temporary relief of pruritus
Intrapartum Management
- FBC and Group & Save
- Clotting profile if bile acids >40
- Due to high risk of fetal distress, close monitoring throughout induction and labour.
- Electronic fetal monitoring is essential throughout labour
- Active management of 3rd stage – risk of PPH if prothrombin time is prolonged
Postnatal Management
- Check LFT’s 10 days post-natal – ensure biochemical abnormalities are resolving
- Resolution of symptoms and LFT’s is required to secure the diagnosis
- High recurrence rate – 45% – 90%
- Discuss effective contraception – avoid oestrogen containing contraceptions
- Increase incidence of obstetric cholestasis in family members
- General Practitioner to ensure LFT’s have returned to normal 12 weeks post delivery
- If LFTS are still abnormal refer to Gastroenterologist
Essential Points for GPs
- Check LFT’s 10 days post-natal – ensure biochemical abnormalities are resolving
- GP to ensure LFT’s have returned to normal 12 weeks post-delivery, If still abnormal to refer to Gastroenterologist
Discuss effective contraception – avoid oestrogen- containing methods
Reference
Royal College of Obstetricians & Gynaecologist. 2011 should be moved from definition heading to under the reference below
