Management of breech presentation
Intrahepatic Cholestasis of Pregnancy / Obstetric Cholestasis
Menopause and Hormone replacement therapy
Management Of Breech Presentation
Dr Maheshie Obeysekera Specialist trainee O&G
Table of content
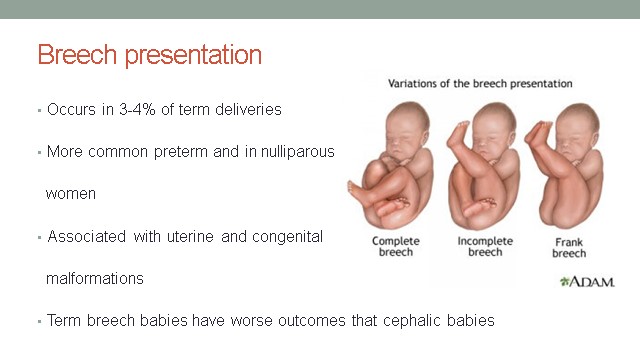
1. Breech Presentation
2. Term Breech Trial (TBT)
3. Criticism of TBT
4. Patient counselling
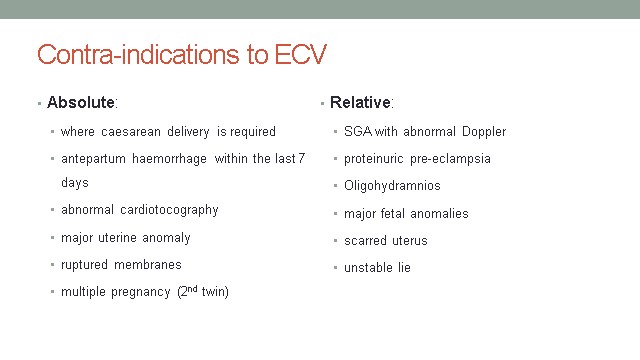
5. ECV-External cephalic version
6. Planned caesarean section
7. Planned Breech delivery
8. Unplanned breech presentation in labour
9. Twin pregnancy with breech presentation
10. Recommendation
11. Reference
Breech Presentation
Term Breech Trial (TBT)
- Randomised 2088 women to either caesarean section or vaginal birth
- Reduction in perinatal mortality with planned caesarean section (1.3 to 0.3%)
- Reduction in the composite outcome of serious neonatal morbidity
- Failed to identify group for whom morbidity was not increased
- 2 year follow-up (923) – no difference in death or neurodevelopmental delay
Criticism of TBT
- 31% had no ultrasound (exclude extended neck)
- Growth restricted babies included
- Woman randomised in violation of protocol
- 9% – senior obstetrician absent, 13% – any obstetrician absent
- EFM not used in most deliveries and prolonged active stage allowed
- Serious neonatal morbidity included benign outcomes
- Caesarean group delivered at 39/40
Other studies
- Dutch study evaluated effect following TBT
- 58320 babies- mortality reduced from 0.13 to 0.07%
- Perinatal mortality – 0.16% vaginal, 0% caesarean
- Caesarean section – reduced risk of low Apgars and neonatal trauma
- 338 extra caesarean sections for each perinatal death prevented
- PREMODA
- 2526 vaginal breech vs 5579 ELLSCS
- Perinatal mortality – 0.12% vaginal, 0.08% caesarean
- No difference in NNU admissions or serious neonatal morbidity
- Increased risk of low Apgars (<7) and fetal injuries
Patient Counselling
- Offer ECV unless contra-indicated
- If unsuccessful or declined – discuss risks and benefits of vaginal breech delivery vs caesarean section
- Inform women of risk of perinatal mortality:
- 0.5/1000 with caesarean section after 39 weeks
- 2.0/1000 with planned vaginal breech birth
- 1.0/1000 with planned cephalic birth.
- Small increase in immediate complications for mother with caesarean sections
- Highest risk is associated with Emergency Caesarean section – needed in 40% of vaginal breech births
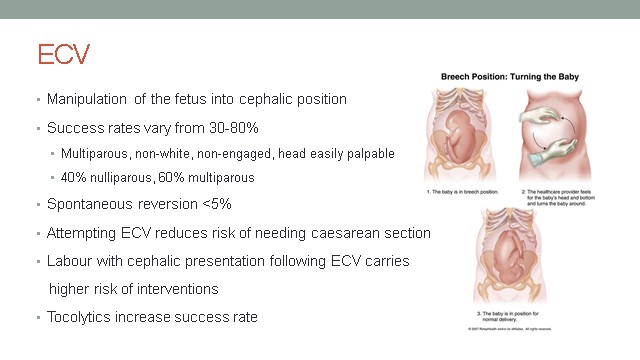
- 36/40 in nulliparous, 37/40 multiparous (no upper time limit)
- Low complication rate
- Placental abruption, uterine rupture, fetomaternal haemorrhage
- 5% Emergency caesarean section rate
- No increase in neonatal morbidity or mortality
- Perform in unit with facilities for fetal monitoring and immediate delivery
- Inform patient that may be painful
Planned Caesarean Section
- Small reduction in perinatal mortality
- avoidance of stillbirth after 39 weeks of gestation
- avoidance of intrapartum risks
- Avoidance of risks of vaginal breech birth
- Small increase in immediate complications for the mother
- Increases the risk of complications in future pregnancies
- Small increase in risk of stillbirth for subsequent pregnancies
- Increases risk of low Apgars and serious short term complications
- No increase in long term complications
Planned Breech delivery
- Safety depends on case selection,
- Risk factors for poorer outcomes: Hyperextended neck on ultrasound, High EFW (> 3.8 kg) or low EFW (< tenth centile), Footling presentation, Evidence of antenatal fetal compromise
Intrapartum Management
- Induction of labour not usually recommended
- Delivery in unit with facilities for immediate caesarean
- Augmentation with oxytocin should only be considered if infrequent contractions with an epidural
- Epidural – effect unclear but likely to increase the risk of intervention
- Continuous Electronic fetal monitoring likely to improve neonatal outcomes
Management of the first stage and passive second stage
- Semi recumbent or an all-fours position may be adopted for delivery
- Allow adequate descent of the breech to the perineum in the passive second stage
- If not visible within 2 hours do caesarean section
Active second stage
- Once buttocks passed perineum – significant cord compression
- ‘Hands off’ approach – tactile stimulation of the fetus may result in reflex extension of the arms or head
- Assistance, without traction, is required if there is a delay or evidence of poor fetal condition
- Grasp around pelvic girdle, not soft tissue
- Back should remain anterior – can use gentle rotation
- Once the scapula is visible, the arms can be hooked down by inserting a finger in the elbow and flexing the arms across the chest
Manoeuvres
- Lovset’s manoeuvre
- Trunk rotated with downward traction so posterior shoulder comes below symphysis pubis. Arm delivered by flexing the shoulder and elbow. Repeated by reverse rotation at 180 degrees to deliver anterior shoulder
- Mauriceau-Smellie-Veit manoeuvre:
- left hand in vagina, palpate the fetal maxilla using the index and middle finger and gently press on the maxilla, bringing the neck to a moderate flexion. The left hand’s palm should rest against the fetus’ chest, while the right hand can grab either shoulder of the fetus and pull in the direction of the fetus’ pelvis
- Suprapubic pressure will aid flexion if there is delay due to an extended neck.
- Bracht manoeuvre: Following spontaneous delivery to the level of the umbilicus, the body is grasped in both hands keeping the legs flexed against the baby’s abdomen and, without traction, is brought up against the symphysis pubis, frequently accompanied by suprapubic pressure
Unplanned breech presentation in labour
- Management depends on stage of labour, presence of risk factors, availability of clinical expertise and informed consent
- If near or in active 2nd stage – should not routinely offer caesarean
- If possible – Ultrasound to assess position of fetal neck and legs + EFW
- Appropriate counselling required
Preterm breech management
- Breech presentation more common
- Studies have shown no significant difference in outcomes
- Caesarean section should not be routinely offered in spontaneous labour or at the threshold of viability (22-25+6)
- Depends on stage of labour, fetal wellbeing and operator skill
- If planned delivery for maternal/fetal compromise – offer caesarean section
Preterm breech – intrapartum management
- Labour should be managed as with a term breech.
- Avoid routine amniotomy
- Trunk may deliver through and incompletely dilated cervix (14%)
- Where there is head entrapment, incisions in the cervix (vaginal birth) or vertical uterine incision extension (caesarean section) may be used
Twin pregnancy with breech presentation
- Recommend caesarean section where presenting twin is breech
- The mode of delivery should be individualised
- Routine Caesarean section is not recommended -If first twin is breech in spontaneous labour or breech presentation of the second twin if first twin is cephalic. The mode of delivery should be individualised based on cervical dilatation, station of the presenting part, type of breech presentation, fetal well being and availability of an operator skilled in vaginal breech delivery
- The chance of cephalic delivery may be improved by guiding the head of the second twin towards the pelvis during and immediately after delivery of the first twin.
- Alternatively delivery of the second twin can be expedited by internal podalic version and breech extraction
Recommendations
- Women should be adequately counselled and give informed consent
- Simulation equipment should be used to rehearse the skills that are needed during vaginal breech birth by all doctors and midwives.
- All obstetricians and midwives should be familiar with the techniques that can be used to assist vaginal breech birth.
- Guidance for the case selection and management of vaginal breech birth should be developed in each department by the healthcare professionals who supervise such births.
- Adherence to the guidelines is recommended to reduce the risk of intrapartum complications.
