Massive Obstetric Haemorrhage
Infertility
Obs & Gynae Yearly Subscription
Massive Obstetric Haemorrhage
Funmi Odusoga DFRSH MRCOG
Table of content
1. Introduction
2. Definition
3. Classification
4. Risk factors
5. Prevention
6. Clinical signs of blood loss
7. Management
8. References
Introduction
- One of the major causes of maternal death both in developed and developing countries
- 3rd highest cause of death in the UK confidential enquiries into maternal deaths 2003-2005
- 58% 10(17) considered preventable
- 7th highest cause in 2011-2013
- Responsible for 50% of maternal death throughout the world
- Incidence 3.7% per 1000 births
Definition
- Definition: Major Obstetric Haemorrhage is defined as blood loss >2000ml or rate of blood loss of 150mls/min, or 50% blood volume loss within 3hrs.
- It may result in a decrease in haemoglobin (Hb) >40g/l, or an acute transfusion requirement of >4 units
- Blood volume depends on the body weight (approximate blood volume equals weight in kilograms divided by 12 expressed as litres). In estimating percentage of blood loss, consideration should be given to body weight and the original haemoglobin
Classification
- Obstetric haemorrhage is classified as antepartum (APH); bleeding occurring after 24 weeks gestation and before delivery,
- (PPH). Postpartum haemorrhage can be primary (within 24 h of delivery) or secondary (24 h to six weeks after delivery).
Risk Factors /Aetiology
Antepartum haemorrhage
- Placenta praevia
- Placental abruption
- Uterine rupture
- Trauma
Primary postpartum haemorrhage
- Uterine atony
- Retained products of conception
- Genital tract trauma
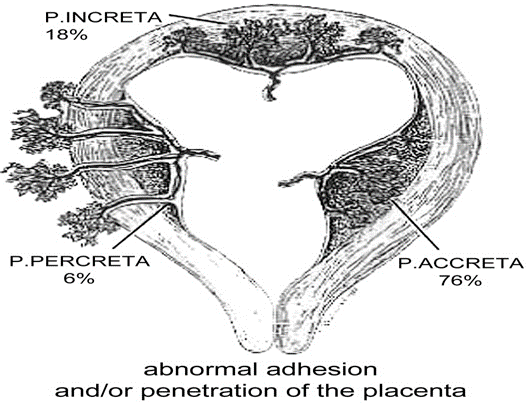
- Abnormally adherent placenta
- Clotting defects
- Acute uterine inversion
- Amniotic fluid embolism
Secondary postpartum haemorrhage
- Puerperal sepsis
- Retained products of conception
Antepartum haemorrhage (APH)
Bleeding from the genital tract in pregnancy ≥24/40 before onset of labour
Causes:
- Maternal
- Unexplained
- Placenta praevia
- Placental abruption
- Fetal: vasa praevia
Primary PPH
| “Blood loss of ≥500 mls from the genital tract within 24 hours of the birth of a baby” |

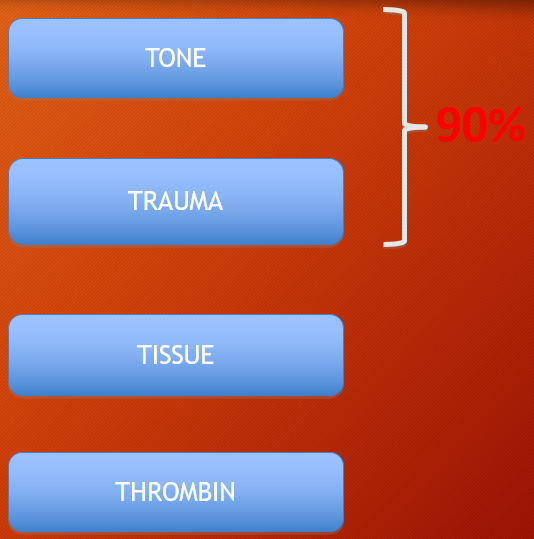
Causes of Primary PPH
PPH Risk Factors
– Maternal age < 20 or>/=40
– Caesarean delivery (+/-‐labour)
– Hypertensive disorders of pregnancy
– Polyhydramnios
– Chorioamnionitis
– Multiple Gestation
– Retained Placenta
– Antepartum Hemorrhage
Prevention
- Active management of 3rd stage of labour reduces the risk of PPH
- Offer routine oxytoxic-60% reduction
- Vaginal delivery 5i.u or 10i.u IM
- Caesarean section 5i.u by slow intravenous injection
- Syntometrine may be used in the absence of HTN-increases vomiting
- Misoprostol –not as effective as oxytocin but may be used in home birth setting when oxytocin is not available
- Placenta site localisation in all women
Clinical Signs Of Blood Loss
- Visible excessive loss (may/not be present)
- Skin pallor & clamminess
- Tachypneoa
- Tachycardia (⇧HR 20% indicates major haemorrhage)
- Altered mental state (agitation, confusion, drowsiness, coma)
- ⇩ BP (late sign)
- Pain (may/not be present)
- Decrease in UO (may be late sign)
Management
- Principles of management
- Communication
- Resuscitation
- Monitoring and investigation
- Arresting the bleeding
(All these must be undertaken simultaneously)
Communication
- Call for help- NEVER HESITATE
- Trigger the massive obstetric haemorrhage protocol bleep
- Experienced midwife in addition to midwife in charge
- Obstetrician
- Anaesthetist
- Haematologist
- Transfusion lab
- Porters
- Scribe to record events, fluids, drugs and vital signs
Use standard form of words e.g We need compatible blood now
Massive Haemorrhage
- Activate ‘Massive Blood Loss’ policy if PPH ≥ 1500mls
- 2222, ‘Emergency Obstetric team’, ask to activate ‘Massive Blood Loss’ protocol, state:
- Your Full Name and Designation
- Hospital Site and Location
- Patients Details
- An appropriate Contact Number for all future communications
- Response team will include
- Obstetric team
- Anaesthetist
- Labour ward practitioners
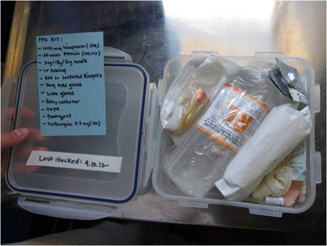
PPH Emergency Box & Resus Trolley

Resuscitation
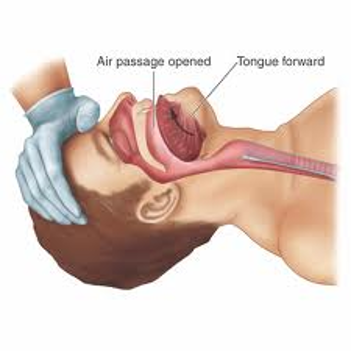
- Assess airway and breathing
- Evaluate circulation
- Oxygen by mask 10-15litres / minute
- 2x 14 gauge cannulae
- Position flat
- Keep warm
- Transfuse blood ASAP
- Infuse 3.5litres of warm hartmann’s as rapidly as required until blood is available
- Recombinant factor VIIa therapy should be based on the results of coagulaion
A B C
- Crystalloid-up to 2litres of hartmann’s solution
- Colloid -1-2litres until blood arrives
- Blood – Crossmatched/O-ve blood
- Fresh frozen plasma – 4units for every 6 units of red cells or PT/APTT > 1.5x normal
- Platelets concentrate- if PLT count < 50
- Cryoprecipitate-if fibrinogen < 1
Monitoring and Investigation
- Venepuncture 20mls
- Crossmatch 4 units minimum
- FBC, COAG including fibrinogen, Renal and liver function baseline
- Monitor temp every 15mins
- Continuous PR,BP, RR,ECG and SATs
- Foleys catheter to monitor urine output
- 2 peripheral cannulae 14 or 16G
- Arterial line monitoring
- Document
- Transfer to HDU / ICU
Venous Access & Bloods




Arresting The Bleeding
- Uterine atony
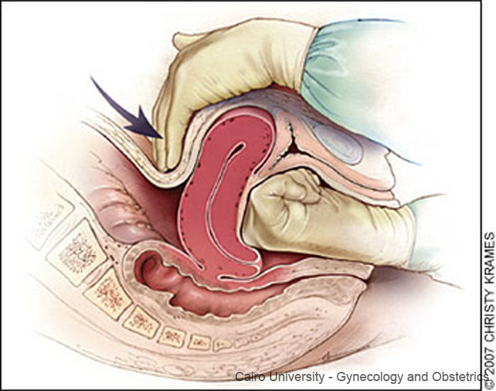
- Bimanual uterine compression
- Empty bladder insert foleys catheter
- Syntocinon by slowIV
- Ergometrine by slow IM/IV avoid in HTN
- Synto infusion 40units in500mls at 125mls/hr
- Carboprost 0.25mg IM at intervals of 15minutes up to 8 doses, avoid in asthma patient
- Misoprostol 1g PR
Bimanual
Surgical
- Suture perineal / cervical tears asap
- Balloon tamponade
- Haemostatic brace suture
- Bilateral ligation of uterine arteries
- Bilateral ligation of internal iliac
- Selective arterial embolization
- HYSTERECTOMY sooner than later especially in placenta accrete or uterine rupture
