Placenta Praevia and Placenta Accreta
Cervical insufficiency/cerclage
Genital Herpes in Pregnancy
Placenta Praevia and Placenta Accreta – Diagnosis and Management
Dr Ayesha Ajmi MRCOG
Table of content
1. Definition/terminology
2. Risk Factors for placenta praevia
3. Antenatal screening
4. Planned delivery
5. Surgical approach in managing placenta praevia
6. Placenta accreta spectrums
7. Risk factor of placenta accreta
8. Antenatal diagnosis of placenta accreta
9. Complications
10. Delivery of placenta accreta
11. Care bundle
12. Surgical approach in placenta accreta
13. Undiagnosed Placenta accreta
14. Risk management
15. References
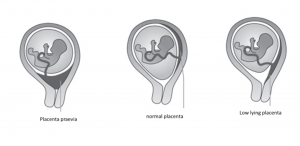
Definition/Terminology by RCOG
- Placenta praevia is defined as placenta lies directly over the internal os
- Low lying placenta: placental edge less than 20 mm from internal os on transabdominal or transvaginal scan after 16 weeks
Risk Factors
- Caesarean delivery
- Maternal smoking
- Assisted reproductive technology
- Rising maternal age
- Short interpregnancy interval after caesarean section
- Prelabour caesarean section
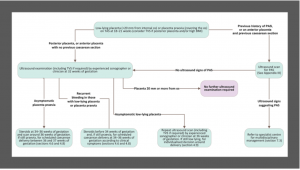
Antenatal screening
- Mid-pregnancy routine fetal anomaly scan 18+6 -21+6 weeks gestation
- Placental localization during anomaly scanning
- Identify women at risk of persisting placenta praevia or low-lying placenta
- Organise follow up scan at 32 weeks for women with either low lying placenta/Placenta praevia
- Transvaginal scan is safe and superior to transabdominal scan
- Asymptomatic women with persistent placenta praevia or low-lying placenta should have a follow up scan at 36 weeks
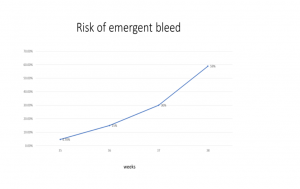
- Short Cervical length at gestational age below 34 weeks increases risk of preterm emergency delivery and massive haemorrhage at caesarean section
- The use of cervical cerclage to reduce bleeding and prolong pregnancy is not supported by sufficient evidence
- Prevent and treat anaemia in all pregnant women

Management of Women with recurrent bleeding
- Tailor hospitalization with individual needs and social circumstances e.g. Distance of home to hospital, Transportation, Previous bleeding episodes
- Check haematology laboratory results
- Discuss acceptance of donor blood or blood products
- Do Risk assessment for VTE and balance against risk of bleeding
Women managed at home should attend hospital immediately;
- If bleeding or Spotting
- Contractions
- Vague suprapubic pain
Antenatal steroids
- Administer single course of steroids at 34-35+6 weeks
- Before 34 weeks; if high risk for preterm delivery
- Tocolysis may be considered for 48 hours to administer steroids
- If delivery is indicated e.g. active bleeding, fetal or maternal compromise, tocolysis should not be used
Planned Delivery
- Uncomplicated placenta praevia: delivery 36-37 weeks
- Vaginal bleeding and risk for preterm delivery: 34-36+6 weeks
Is Vaginal delivery appropriate for women with a low-lying placenta?
When placenta edge is between 10-20mm from the internal os success rates of vaginal delivery varies widely from 56%-93% (From small retrospective and observational studies)
In women with a third trimester asymptomatic low- lying placenta the mode of delivery should be based on
- Maternal preference
- Thickness of placental edge
- Position of head in relation to lower edge of placenta
Optimising delivery
- Discussion about blood transfusion and hysterectomy
- Placenta praevia and anterior low-lying placenta carry high risk of Massive Obstetric Haemorrhage therefore delivery should be in a maternity with on-site blood transfusion services, Access to critical care
- Women with atypical antibodies: discuss with blood bank and haematologist
Delivery
- Should be performed by appropriately experienced operator
- Senior Obstetrician (Usually Consultant) and senior anaesthetist usually consultant must be present in theatre suite
- Consultants obstetrician and anaesthetist should be Alerted immediately and attend urgently when an emergency arises
- Regional anaesthesia is appropriate and safe
- Consent patient for conversion to GA if required
Blood products
- Close liaison with the hospital transfusion laboratory
- Cell salvage
- Rapid infusion and fluid warming devices should be immediately available
Surgical approach in managing Placenta praevia
- Vertical incision: transverse lie and less than 28 weeks
- Ultrasound to determine optimal place for uterine incision
- If placenta transected, immediately clamp umbilical cord to minimize blood loss
- Pharmacological measures-syntocinon, syntometrine, carbaprost, misoprostol
- intrauterine tamponade e.g. Bakri Balloon
- Surgical haemostatic techniques e.g. B-Lynch brace sutures, uterine artery ligation, internal iliac ligation
- Early recourse to hysterectomy
Placenta Accreta spectrum
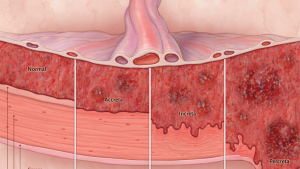
Risk factors for Placenta Accreta
- History of accreta in previous pregnancy
- History of caesarean delivery
- No. of previous caesareans
- History of prelabour caesarean section: 3 times more likely (Kamara et al 2013)
- Other uterine surgery
- Repeated uterine curettage
- Previous caesarean and anterior low lying or placenta praevia
- Risk rises as the number of prior caesarean sections increases
Antenatal Diagnosis of placenta accrete spectrum
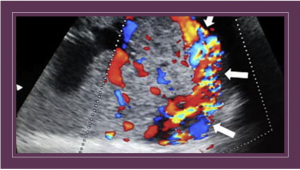
- Ultrasound is highly accurate when performed by a skilled operator-Uterus bladder interface, abnormal vasculature, placental lacunae, moth eaten appearance and increased vascularity of placental bed
- MRI scan (also used to compliment ultrasound) shows the depth of invasion and lateral extension of myometrial invasion Abnormal uterine bulge, dark intraplacental bands on T2-weighted imaging, heterogeneous signal intensity within the placenta, disorganised vasculature of placenta and disruption of the uteroplacental zone

Complications
- Hamorrhage and hysterectomy
- Placenta percreta: uterine rupture and bladder involvement
Delivery of placenta accrete
- If there is no risk factors for preterm delivery deliver between 35-36+6 weeks
- Make contingency plan with woman
- Discuss Institutional protocol for massive haemorrhage with woman
- Take Consent and discuss massive obstetric haemorrhage, increased risk of lower urinary tract damage, the need for blood transfusion and the risk of hysterectomy.
- Discuss Cell salvage and Interventional radiology where available
- Regional anaesthesia may require conversion to general anaesthesia
- Caesarean hysterectomy is preferable when compared to attempt to separate placenta
- Consider Uterus preserving surgery: partial myometrial resection if extent is limited
- Placenta percreta hysterectomy
- Placenta left in situ: bleeding and infection
- Methotrexate not recommended
- Ureteric stents if bladder involved
Care bundle
- Consultant obstetrician planning and directly supervising delivery.
- Consultant anaesthetist planning and directly supervising anaesthesia at delivery.
- Blood and blood products availability.
- Multidisciplinary involvement in preoperative planning.
- Discussion and consent, including possible interventions (such as hysterectomy, leaving the placenta in salvage and interventional radiology).
- Local availability of a level 2 critical care bed.
Surgical approach in placenta accreta
- Primary hysterectomy without attempting placental separation
- Delivery of the fetus avoiding the placenta, with repair of the incision leaving placenta in situ
- Delivery of the fetus without disturbing the placenta, followed by partial excision of the uterine wall (placental implantation site) and repair of the uterus.
- Delivery of the fetus without disturbing the placenta, and leaving it in situ, followed by elective secondary hysterectomy 3–7 days following the primary procedure.
Undiagnosed placenta accreta
- Undiagnosed placenta percreta-Delay delivery if possible until resources available
- You may need to close abdomen and transfer to specialist unit
- Where appropriate leave placenta in situ after delivery
- Emergency hysterectomy
Risk Management
- Debriefing
- Training
- Incident reporting
Reference
- Placenta Praevia and Placenta Accreta: Diagnosis and management-Green-top Guideline No. 27a September 2018
