Thalassemia in Pregnancy
Endometriosis
Contraception and family planning
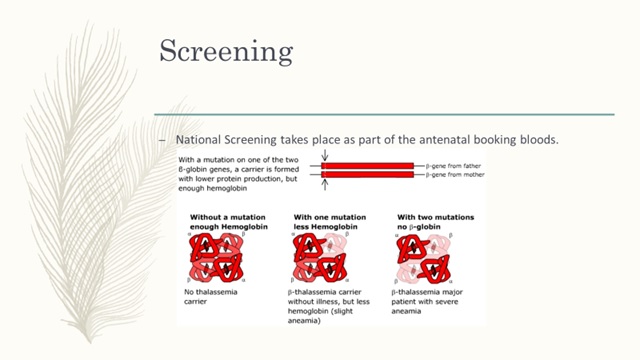
Table of content
1. Introduction
2. Types
3. Screening
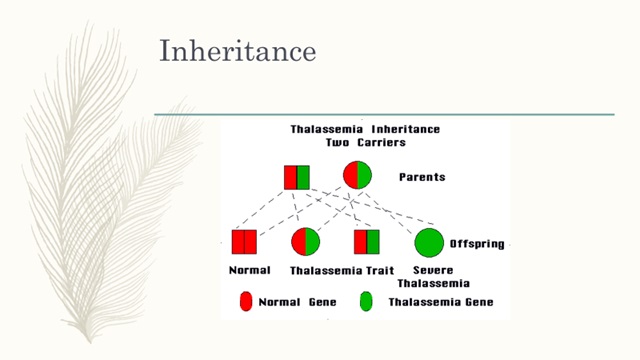
4. Inheritance
5. Preconception care
6. Antenatal care
7. Intrapartum care
8. Postnatal care
9. References
Introduction
- A type of haemoglobinopathy
- More than 70 000 babies are born with thalassaemia worldwide each year
- 100 million individuals who are asymptomatic thalassaemia carriers.
- There is reduced globin chain synthesis with the resultant red cells having inadequate haemoglobin content.
- The pathophysiology of thalassaemia syndromes is characterised by extravascular haemolysis due to the release into the peripheral circulation of damaged red blood cells and erythroid precursors because of a high degree of ineffective erythropoiesis.
Types
- Thalassaemia major (homozygous Β thalassaemia) results from the inheritance of a defective β-globin gene from each parent. This results in a severe transfusion-dependent anaemia.
- The heterozygous state, β thalassaemia trait (thalassaemia minor) causes mild to moderate microcytic anaemia with no significant detrimental effect on overall health.
- Thalassaemia intermedia is defined as a group of patients with β thalassaemia whose disease severity varies.
Preconception care
- Use of contraception is advised if no intention on pregnancy
- (Thalassaemia can reduce fertility if iron overload damages the anterior pituitary may require gonadotrophin injections to help conception)
- MDT care (including obstetrician, haematologist)
- Screening of end-organ damage
- Iron chelation therapy
- 5mg folic acid 3 months prior to conception
Medications to stop
- Iron chelators should be reviewed and deferasirox and deferiprone ideally discontinued 3 months before conception.
- Bisphosphonates should be discontinued 3 months before conception.
Genetic screening
- If the partner is a carrier of a haemoglobinopathy that may adversely interact with the woman’s genotype then genetic counselling should be offered.
- In vitro fertilisation/intracytoplasmic sperm injection (IVF/ICSI) with a pre-implantation genetic diagnosis (PGD) should be considered in the presence of haemoglobinopathies in both partners so that a homozygous or compound heterozygous pregnancy can be avoided.
- Egg and sperm donors considering IVF should be screened for haemoglobinopathies.
Risk of hepatitis B&C - Hepatitis B vaccination is recommended in HBsAg negative women who are transfused or may be transfused.
- Hepatitis C status should be determined.
- All women who have undergone a splenectomy should take penicillin prophylaxis or equivalent.
- All women who have undergone a splenectomy should be vaccinated for pneumococcus and Haemophilus influenzae type b if this has not been done before.
Antenatal Care
- Women with thalassaemia should be reviewed monthly until 28 weeks of gestation and fortnightly thereafter. The multidisciplinary team should provide routine as well as specialist antenatal care.
- Women with both thalassaemia and diabetes should have monthly assessment of serum fructosamine concentrations and review in the specialist diabetic pregnancy clinic.
- All women with thalassaemia major should undergo specialist cardiac assessment at 28 weeks of gestation and thereafter as appropriate.
- Thyroid function should be monitored during pregnancy in hypothyroid patients.
- Iron chelation therapy as per individual needs
Thromboprophylaxis
- Women with thalassaemia who have undergone splenectomy or have a platelet count greater than 600 x 109/l should commence or continue taking low-dose aspirin (75 mg/day).
- Women with thalassaemia who have undergone splenectomy and have a platelet count above 600 x 109/l should be offered low-molecular-weight heparin thromboprophylaxis as well as low-dose aspirin (75 mg/day).
- Women with thalassaemia who are not already using prophylactic low-molecular-weight heparin should be advised to use it during antenatal hospital admissions.
Ultrasound schedule
- Early USS (7-9 weeks’ gestation)
- Dating USS at 12 weeks
- Anomaly scan
- Growth scans every 4 weeks from 24 weeks-(Risk of IUGR due to severe maternal anaemia)
Blood transfusion
- All women with thalassaemia major should be receiving blood transfusions on a regular basis aiming for a pre-transfusion haemoglobin of 100 g/l.
Intrapartum care
- Timing of delivery is dependent on individual circumstances such as suspected IUGR or worsening cardiomyopathy
- CTG monitoring-Electronic fetal monitoring
- Active 3rd stage to minimise blood loss
- Group and save blood or cross-match 2 units if evidence of antibodies
- In women with thalassaemia major intravenous desferrioxamine 2 g over 24 hours should be administered for the duration of labour.
- Inform senior obstetrician and haematologist when lady is admitted to delivery suite
Postnatal
- High risk of VTE so thromboprophylaxis is recommended – 7 days post NVD or 6 weeks post Caesarean section
- Breastfeeding is safe and recommended
- Women with thalassaemia major who plan to breastfeed should restart Desferrioxamine as soon as the initial 24-hour infusion of intravenous Desferrioxamine finishes after delivery. Desferrioxamine is secreted in breast milk but is not orally absorbed and therefore not harmful to the new-born. There is minimal safety data on other iron chelators.
- If a woman decides not to breastfeed, intravenous or subcutaneous Desferrioxamine infusions are continued until discharge from hospital or until resumption of her previous iron chelation regimen under haematology supervision, whichever is sooner
- Check baby’s haemoglobinopathy screen on a cord sample
- Ensure follow up in a Obstetric haematology clinic
References
1. Management of Beta Thalassaemia in Pregnancy: Green-top Guideline No. 66 (March 2014)
2. https://thalnsw.org.au/?q=content/what-thalassaemia
3. http://www.thalassemia.org/boduw/wp-content/uploads/2016/08/MRI-in-Thalassemia.pdf
4. Management of Major Haemoglobinopathy in Pregnancy, Bolton Hospital guidelines, 2016
