Third and Fourth degree perineal tear
Chronic kidney disease in pregnancy
Management of common Obstetric Emergencies
Third and Fourth degree perineal tear
Table of content
1. Introduction
2. Classification
3. Risk factors
4. Prevention
5. Identification
6. Repair
7. Post-operative management
8. Prognosis
9. Future deliveries
10. References
Introduction and background epidemiology
- The overall incidence in the UK is 2.9% (range 0–8%), with an
- incidence of 6.1% in primipara compared with 1.7% in multiparae.2
- With increased awareness and training, there appears to be an increase in the detection of anal sphincter
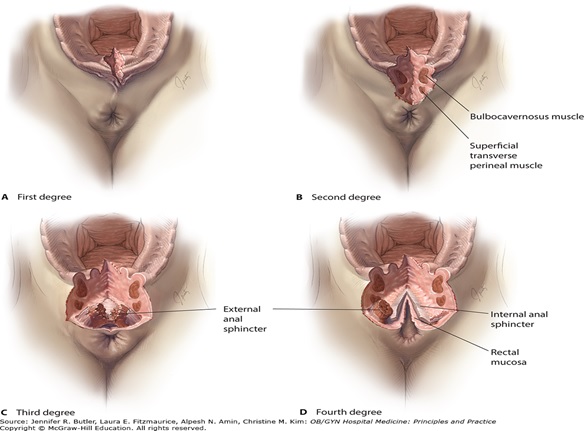
Classification
- If there is any doubt about the degree of third-degree tear, it is advisable to classify it to the higher degree rather than the lower degree
- First-degree tear: Injury to perineal skin and/or vaginal mucosa.
- Second-degree tear: Injury to perineum involving perineal muscles but not involving the anal
sphincter
- Third-degree tear: Injury to perineum involving the anal sphincter complex:
- Grade 3a tear: Less than 50% of external anal sphincter (EAS) thickness torn.
- Grade 3b tear: More than 50% of EAS thickness torn.
- Grade 3c tear: Both EAS and internal anal sphincter (IAS) torn.
- Fourth-degree tear: Injury to perineum involving the anal sphincter complex (EAS and IAS) and anorectal mucosa.
- Obstetric anal sphincter injuries (OASIS) encompass both third- and fourth-degree perineal tears
- Anal incontinence is defined as the complaint of involuntary loss of flatus and/or faeces affecting quality of life
- Rectal buttonhole tear-If the tear involves the rectal mucosa with an intact anal sphincter complex, it is by definition not a fourth-degree tear. This has to be documented as a rectal buttonhole tear. If not recognised and repaired, this type of tear may lead to a rectovaginal fistula
Risk factors for Third and Fourth degree tear
- Asian ethnicity1(OR 2.27, 95% CI 2.14–2.41)
- Nulliparity15 (relative risk [RR] 6.97, 95% CI 5.40–8.99)
- Birthweight greater than 4 kg1 (OR 2.27, 95% CI 2.18–2.36)
- Shoulder dystocia(OR 1.90, 95% CI 1.72–2.08)
- Occipito-posterior position15 (RR 2.44, 95% CI 2.07–2.89)
- Prolonged second stage of labour
Duration of second stage between 2 and 3 hours (RR 1.47, 95% CI 1.20–1.79)
Duration of second stage between 3 and 4 hours (RR 1.79, 95% CI 1.43–2.22)
Duration of second stage more than 4 hours (RR 2.02, 95% CI 1.62–2.51)
- Instrumental delivery:1
Ventouse delivery without episiotomy (OR 1.89, 95% CI 1.74–2.05)
Ventouse delivery with episiotomy (OR 0.57, 95% CI 0.51–0.63)
Forceps delivery without episiotomy (OR 6.53, 95% CI 5.57–7.64)
Forceps delivery with episiotomy (OR 1.34, 95% CI 1.21–1.49).
Risk factors for OASIS were assessed in a retrospective study of 123
(Williams A, Tincello DG, White S, Adams EJ, Alfirevic Z, Richmond DH. Risk scoring system for prediction of obstetric anal sphincter injury. BJOG 2005; 112:1066–9.)
Prevention of obstetric anal sphincter injury
- Mediolateral episiotomy should be considered in instrumental deliveries.
- Where episiotomy is indicated, the mediolateral technique is recommended, with careful attention to ensure that the angle is 60 degrees away from the midline when the perineum is distended
- Perineal protection at crowning can be protective
- Warm compression during the second stage of labour reduces the risk of Obstetric Anal Sphincter Injuries OASIS
Identification of OASIS
- Administer analgesia e.g. Gas on air, local anaesthetic or regional anaesthesia
- Ensure adequate lighting
- Keep patient in Lithotomy position
- You must perform both vaginal and rectal examination with adequate lighting
- Escalate to a more experienced clinician if uncertainty exists as to extent or nature of trauma sustained
Repair of OASIS
- Should be done by an experienced clinician or under the supervision of an experienced clinician
- Should be done in theatre to ensure appropriate instruments, adequate light and an assistant
- Figure of eight sutures should be avoided during the repair of OASIS because they are haemostatic in nature and may cause tissue ischaemia.
- A rectal examination should be performed after the repair to ensure that sutures have not been inadvertently inserted through the anorectal mucosa. If a suture is identified it should be removed
Techniques of repair-Repair should be done by a competent surgeon
- The torn anorectal mucosa should be repaired with sutures using either the continuous or interrupted technique.
- Where the torn Internal Anal Sphincter can be identified, it is advisable to repair this separately with interrupted or mattress sutures without any attempt to overlap the IAS.
- For repair of a full thickness External Anal Sphincter tear, either an overlapping or an end-to-end (approximation) method can be used with equivalent outcomes.
- For partial thickness (all 3a and some 3b) tears, an end-to-end technique should be used.
Suture materials
- 3-0 polyglactin should be used to repair the anorectal mucosa as it may cause less irritation and discomfort than polydioxanone (PDS) sutures.
- When repair of the EAS and/or IAS muscle is being performed, either monofilament sutures such as 3-0 PDS or modern braided sutures such as 2-0 polyglactin can be used with equivalent outcomes.
- When obstetric anal sphincter repairs are being performed, the burying of surgical knots beneath the superficial perineal muscles is recommended to minimise the risk of knot and suture migration to the skin
Post-operative management
- The use of broad-spectrum antibiotics is recommended following repair of OASIS to reduce the risk of postoperative infections and wound dehiscence.
- The use of postoperative laxatives is recommended to reduce the risk of wound dehiscence.
- Bulking agents e.g. Fybogel should not be given routinely with laxatives.
- Follow up in postnatal clinic 6-12weeks after delivery by a clinician with special interest in OASIS
- Physiotherapy after repair is beneficial
- Refer to colorectal surgeon/specialist gynaecology if patient has incontinence or pain at follow up
Prognosis
- 60–80% of women are asymptomatic 12 months following delivery and EAS repair.
Future deliveries
- The risk of sustaining a further third- or fourth-degree tear after a subsequent delivery is 5–7%
- The risks of a subsequent vaginal delivery after a third degree tear have been assessed, with 17% of women developing worsening faecal symptoms after a second vaginal delivery .This seemed to occur if there had been faecal incontinence beyond 3 months but resolution by 6 months after the index delivery
- All women who sustained OASIS in a previous pregnancy should be counselled about the mode of delivery and this should be clearly documented in the notes.
- The role of prophylactic episiotomy in subsequent pregnancies is not known and therefore an episiotomy should only be performed if clinically indicated.
- Consider caesarean sections deliveries in women who are symptomatic after OASIS repair
References
- Thiagamoorthy G, Johnson A, Thakar R, Sultan AH. National survey of perineal trauma and its subsequent management in the United Kingdom. Int Urogynecol J 2014; 25:1621–7.
- RCOG green top guideline No29 2015
